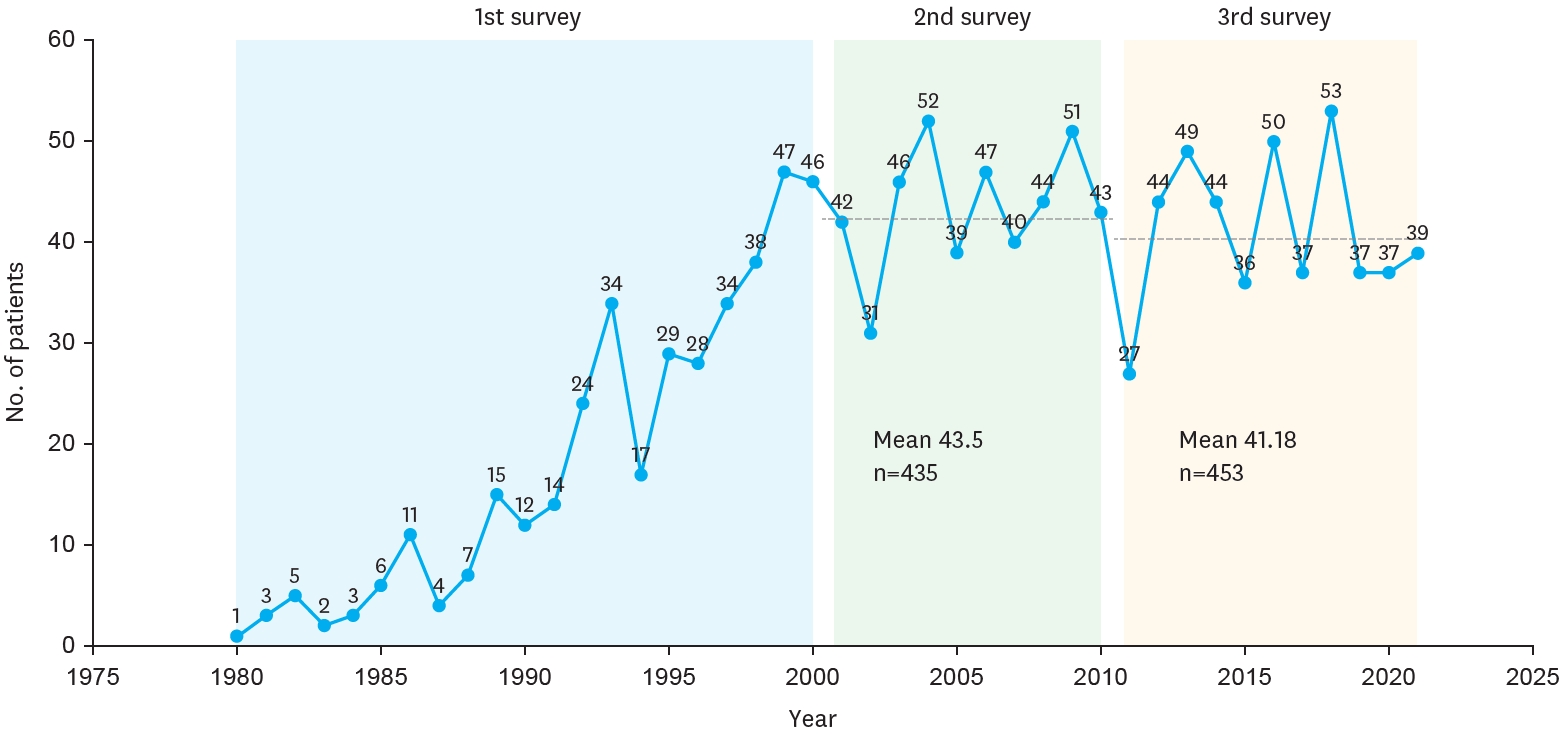
The Korean Association of Pediatric Surgeons (KAPS) performed a nationwide survey on sacrococcygeal teratoma in 2018.
The authors reviewed and analyzed the clinical data of patients who had been treated for sacrococcygeal teratoma by KAPS members from 2008 to 2017.
A total of 189 patients from 18 institutes were registered for the study, which was the first national survey of this disease dealing with a large number of patients in Korea. The results were discussed at the 34th annual meeting of KAPS, which was held in Jeonju on June 21–22, 2018.
We believe that this study could be utilized as a guideline for the treatment of sacrococcygeal teratoma to diminish pediatric surgeons' difficulties in treating this disease and thus lead to better outcomes.
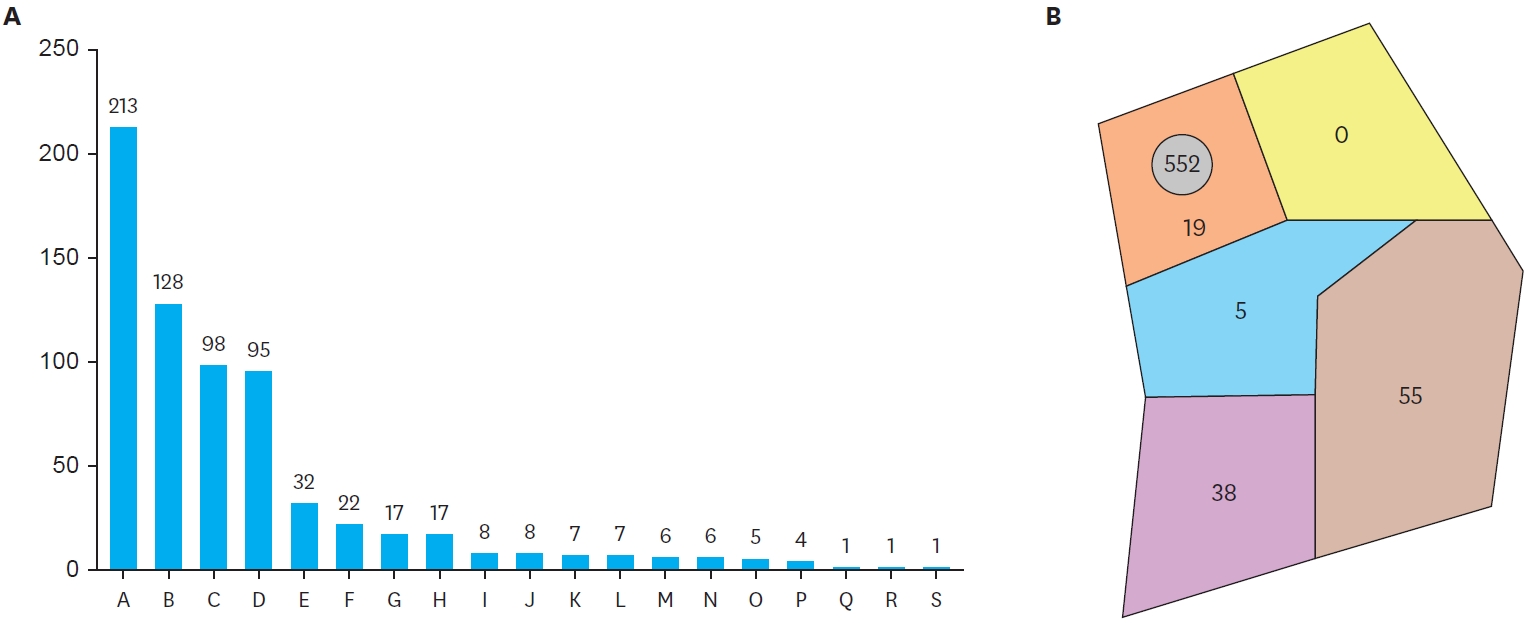
Foreign body ingestion is a common problem among paediatric populations. Most of the ingested foreign bodies spontaneously pass through the gastrointestinal tract, but approximately less then 10% of them remain without being discharged, and trigger complications. Therefore, proper evaluation and treatment according to the situation is required. In this study, clinical progress and complications were analyzed according to the clinical features and treatment in children who ingested foreign bodies. Among pediatric patients under 18 who were admitted to Chonnam National University Hospital after ingesting foreign bodies between January 2008 to June 2012, only the patients who had their foreign body in the gastrointestinal tract were included in this study. Based on medical records, age, type of foreign body, time spent till admission, and whether the endoscopy was done or not, complication were researched retrospectively. According to symptoms and plain abdomen X-ray findings, treatment was chosen and conducted among endoscopy, observation and emergency operation. Among 273 patients, 9 (3.3%) of them had surgical removal. Seven (2.6%) of them had an emergency operation on the day of admission, and the rest 2 (0.7%) had operation during observation. Removal through initial endoscopic approach was tried in 157 (57.5%) patients. Eleven (70.8%) of them had their foreign body removed at the initial trial, and 5 (4.9%) of them at the second trial. Among 109, who were on observation status, 9 (8.3%) of them needed endoscopic removal, and 2 (1.8%) of them suffered from surgical removal. It is thought to be better to approach slowly considering the type, size and symptoms in foreign body ingestion of pediatric patients, rather than immediate and invasive removal.
Splenic abscess is a rare clinical condition with a reported incidence of 0.14 % to 0.70 % in various autopsy series. Primary tuberculosis of the spleen as a cause of splenic abscess is even rarer, especially in the antitubercular era. Infants and children have a higher predisposition to extra-pulmonary tuberculosis than adults and tend to develop severe extra-pulmonary disease such as miliary tuberculosis and meningitis. The diagnosis of tuberculosis in infants and children can be difficult because of nonspecific symptoms and clinical findings. Computed tomography establishes the diagnosis of splenic abscess and demonstrates the number and location of abscesses. Splenectomy is the standard of care in most clinical setting. We present a 4-year-old girl who had multiple tuberculosis splenic abscesses and was treated successfully with splenectomy.
The teratoma is a unique complex neoplasm and is one of the most frequent pediatric tumors originated from the extragonadal germ cells. Mature teratoma is composed of mature differentiated tissues, while immature teratoma always contains embryonic tissues of variable degrees of immaturity, especially in the neuroepithelial elements. Diagnosis of teratoma is relatively easy by conventional radiologic study, but the immaturity can be identified only by histopathological examination. Between January 1993 to December 2002, 63 cases of teratoma were operated and analysed retrospectively at the Chonnam University Hospital Female to male ratio was about 3:1 and age distribution was relatively even. Among 63 cases, gonadal teratoma was the most common (52.4%), followed by sacrococcygeal (25.4%), retroperitoneal (9.5%) and mediastinal teratoma (9.5%). Fifty-six cases were mature teratomas and seven were immature teratomas. Alpha-fetoprotein (AFP) was elevated in 4 of 6 immature cases, but in 2 of 51 mature ones Elevated AFP progressively returned to normal range by 1 month after operation in all. Complete excision of the mass was performed, and major complication was not noticed. In five immature cases, PEB chemotherapy (Cisplatin, Etoposide, Bleomycin) was performed. Two of 2 cases in histological grade II were well tolerated to the aggressive chemotherapy. One of three cases in grade III expired due to severe bone marrow depression, and two of them expired by tumor recurrences. In conclusion, immature teratoma in histological grade III showed high potentiality of recurrence. Therefore, postoperative chemotherapy has to be applied to the high graded immature tumors.
Gastroduodenal intussusception, an invagination of a part of the gastric wall through the pyloric canal into the duodenum is a rare condition. Gastroduodenal intussusception is caused by a mobile usually benign gastric tumor. However, gastroduodenal intussusception by gastric submucosal hemangiomatosis is not documented. We have managed a case of gastric submucosal tumor leading to gastroduodenal intussusception in 2 years and 10 months old boy. The tumor was 10 × 5 × 3 cm in size in posterior wall of gastric antrum. Laparotomy, manual reduction of the intussusception, and wedge resection of posterior gastric wall including the tumor were performed. Pathologic diagnosis was a submucosal hemangiomatosis.
This is a clinical review of 2,191 pediatric surgical patients under the age of 15 years, operated upon at the Division of Pediatric Surgery, Department of Surgery, Chonnam University Hospital from January 1988 to December 1997. The total number of operations in the pediatric age for all specialties were 13,144(13.2 %). The total operations including those performed on adults were 99,555. The most common age group operated upon was under 5 year of age(44.4 %). The number of operations in Division of General Pediatric Surgery were 2,191(16.7 %) out of total 13,144 operations in all pediatric specialties. The patients under 1 year of age in general pediatric surgery was 42.9 %(941/2,191). The most common diseases in neonates were anorectal malformation(20.6 %) and hypertrophic pyloric stenosis( 20.3 %). Infants older than neonates most commonly were operated upon for inguinal hernia(32.4 %) and intussusception(19.6 %). The total mortality rate in the neonatal intensive care unit was 31.3 %. Gastroschisis had the highest mortality.
Conjoined twins are one of the rarest and most challenging congenital anomalies in pediatric surgery. Successful surgical separation is difficult because it the majority of conjoined twins in is technically typical to separate shared vital organs successfully. The timing of separation is variable, but separation is usually delayed until such infants are relatively mature(i.e, 9-12 months of age). Operative survival was 50 % in the neonatal period, but 90 % in those over 4 months of age. The present case was successfully separated early beacase of cardiac problems in one of the twins. These twins were omphalopagus and only the liver was shared through a bridge. The vascular and biliary trees were independent from each other. Successful surgical separation was on 11th day of life, but one died of sepsis 18 days ofter operation.

