Citations

The Korean Association of Pediatric Surgeons (KAPS) performed a nationwide survey on sacrococcygeal teratoma in 2018.
The authors reviewed and analyzed the clinical data of patients who had been treated for sacrococcygeal teratoma by KAPS members from 2008 to 2017.
A total of 189 patients from 18 institutes were registered for the study, which was the first national survey of this disease dealing with a large number of patients in Korea. The results were discussed at the 34th annual meeting of KAPS, which was held in Jeonju on June 21–22, 2018.
We believe that this study could be utilized as a guideline for the treatment of sacrococcygeal teratoma to diminish pediatric surgeons' difficulties in treating this disease and thus lead to better outcomes.
Citations

A 6-year-old male who lived with a mother in a single-parent family was referred to the emergency room with multiple traumas. There was no specific finding on CT scan of the other hospital performed 55 days before admission. However, CT scan at the time of admission showed common bile duct (CBD) stenosis, proximal biliary dilatation and bile lake formation at the segment II and III. Endoscopic retrograde biliary drainage was performed, but the tube had slipped off spontaneously 36 days later, and follow-up CT scan showed aggravated proximal biliary dilatation above the stricture site. He underwent excision of the CBD including the stricture site, and the bile duct was reconstructed with Roux-en-Y hepaticojejunostomy. Pathologic report of the resected specimen revealed that the evidence of trauma as a cause of bile duct stricture. While non-iatrogenic extrahepatic biliary trauma is uncommon, a level of suspicion is necessary to identify injuries to the extrahepatic bile duct. The role of the physicians who treat the abused children should encompass being suspicious for potential abdominal injury as well as identifying visible injuries.
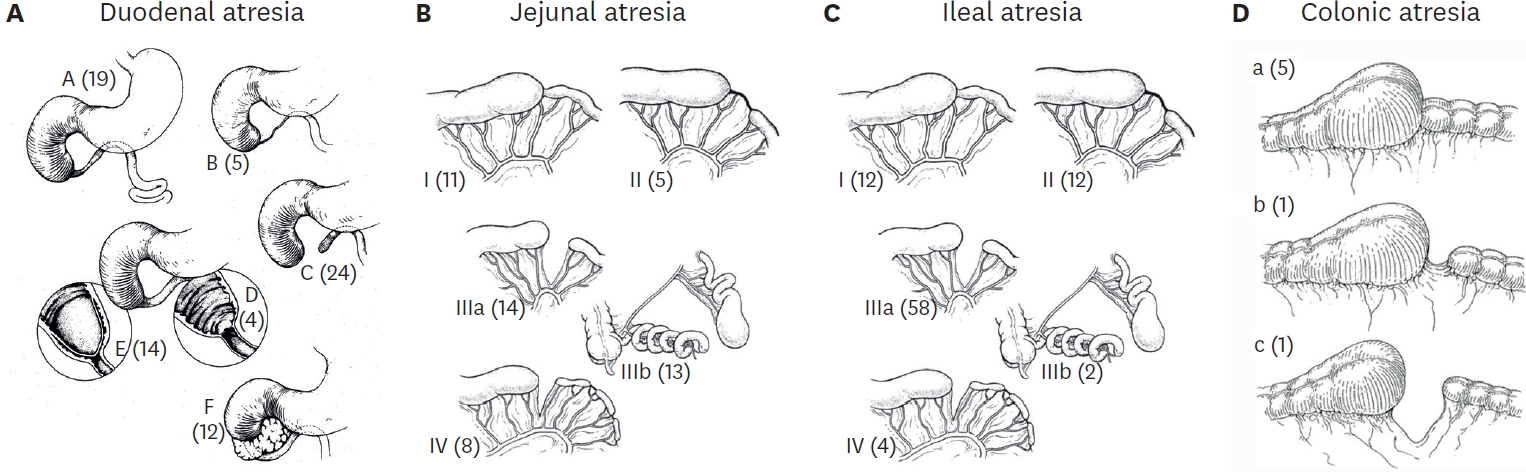
Santulli enterostomy has been used for various surgical abdominal conditions that require temporary diversion of bowel during a neonatal period. The aim of this study was to report clinical outcomes of Santulli enterostomy and to evaluate its usefulness.
Between January 2000 and December 2016, 40 neonates who underwent Santulli enterostomy were enrolled; Santulli enterostomies were performed for 25 patients without previous laparotomy (primary Santulli group) and 15 patients with previous laparotomy (secondary Santulli group).
Small bowel atresia is the first common indication of Santulli enterostomy (22/40, 55.0%), and luminal discrepancy between proximal and distal bowel was the most common determinant factor of Santulli enterostomy (17/40, 42.5%). The median age at surgery and mean birth weight were 2 days and 2,480 g respectively in the primary group, and 71 days, 2,340 g respectively in the secondary group. Operation time was significantly longer in the secondary group than the primary group (156±48 minutes vs. 224±95 minutes, p=0.019), and there was no difference in the time taken to initiation of oral feeding between the two groups. Santulli enterostomy closure was performed at median 65 days after Santulli enterostomy for primary group and 70 days for secondary group. Six complications (15.0%) were found after Santulli enterostomy, and nine complications (24.3%) after Santulli enterostomy closure (p=0.302). The incidence of complications was significantly higher in secondary group than in primary group (4.5% vs. 53.3%, p=0.001), and the reoperation rate was also significantly higher in the secondary group (4.5% vs. 46.7%, p=0.004).
Santulli enterostomy could be applied as a temporary enterostomy in neonatal patients with various surgical abdominal diseases. Considering the high complication rate after secondary Santulli enterostomy closure, decision making on the timing of enterostomy closure should be done with caution.
Citations

In one-stage transanal endorectal pull-through operation (TERPT) for Hirschsprung disease, preoperative evaluation by contrast enema (CE) is important tool in aspect of planning of surgical procedure as well as diagnosis. This study was to evaluate the significance of CE for identifying the extent of aganglionic bowel. A retrospective analysis was performed in 40 patients who underwent TERPT between 2003 and 2011. The authors reviewed the CE studies and their correlation with pathologic extent of aganglionosis. Total 66 contrast enemas were performed in 40 patients. Twenty patients underwent single CE, but 20 patients required multiple CEs. In single CE group, 17 had clear radiographic transition zone, but 3 had less definite transition zone. In multiple CE group, 17 patients who had equivocal finding in first or second CE had definite radiographic transition zone, but 3 patients of this group had less definite radiographic transition zones. Overall, 34 patients (85%) had clear radiographic transition zone by single or repeated CE. One (2.9%) out of 34 patients with clear radiographic transition zone had discordance between radiographic and pathologic transition zone. In contrast 4 (66.7%) out of 6 patients with equivocal radiographic transition zone had discordance between radiographic and pathologic transition zone. Observation of clear radiographic transition zone is important in preparation of TERPT, and repeated CE is helpful to reduce the discordance between radiographic and pathologic transition zone. Awareness of the possibility of discordance is also important if radiographic transitional zone is not clear.
Hiatal hernia is a very rare disease in the pediatric population. However information from our esophageal atresia postoperative follow-up program has hypotheses; “Hiatal hernia may more frequently occur in postoperative esophageal atresia patients (EA group) than in the general pediatric population (GP group)” and “The tension on the esophagus after esophageal anastomosis may be an important etiologic factor of hiatal hernia in EA group”. To prove the first hypotheses, we compared the incidence of hiatal hernia in the GP group with the incidence in the EA group. The Incidence in the GP group was obtained from national statistic data from Statistics Korea and Health Insurance Review and Assessment Service of Korea. The incidence in the EA group was obtained from the medical record and the imaging studies of our esophageal atresia postoperative follow-up program. To prove the second hypothesis, the presumptive risk factors for the development of hiatal hernia in EA group, such as the type of esophageal atresia, degree of esophageal gap, the stage operation and the redo-operation with resection and re-anastomosis of esophagus were analyzed statistically. The total number of patients in the EA group was ninety-nine and there were 5 hiatus hernias. The incidence of EA group (5 %) is significantly higher than incidence of GP group (0.024 %). (
Citations

Although laparoscopic surgery for hepatobiliary disease in children is possible, it is technically challenging. In an attempt to overcome these difficulties, the da Vinci Robotic Surgical System(R) was used to facilitate the minimally invasive treatment of choledochal cyst in six children. In early consecutive three cases, we experienced three complications; a case of laparotomy conversion, a case of late stenosis of the hepaticojejunostomy, and a case of leakage from a hepaticojejunostomy. However, in the last three cases the complete resection of the choledochal cyst and Roux-en-Y hepaticojejunostomy were performed using the robotic surgical system without complication.
We think robot-assisted choledochal cyst resection in children appears safe and feasible, and may increase the variety of complex procedures in pediatric surgical fields.
Citations

Meconium obstruction (MO) in neonates arises from highly viscid meconium and the poor motility of the premature gut. Recently the incidence of the MO in neonates has been increasing, but, the diagnosis and treatment of this disease have not yet been clarified. Between March 2004 and April 2010, 24 neonates were treated for MO at Severance Children's Hospital. Their clinical characteristics and treatment were reviewed retrospectively. Twenty neonates were diagnosed with MO and 4 neonates were diagnosed with Hirschsprung's disease (HD). The mean birth weight and gestational age of the 20 neonates with MO were 1.45±0.90kg and 31.1±4.6 weeks, respectively. Thirteen neonates (65%) diagnosed with MO weighed less than 1.5kg and 10 neonates (50%) weighed less than 1kg. Half of the neonates with MO were treated by non-operative methods and the other half were treated by operative methods. Compared with the group that weighed over 1.5kg, the group that weighed less than 1.5kg were more frequently operated upon (61.5% vs. 28.5%), and contrast enemas were performed later and more frequently. Also the group that weighed less than 1.5kg had a higher mortality rate (15.4% vs. 0%). Three of the four neonates with HD were diagnosed with long-segment aganglionosis. In conclusion, MO occurred in very low birth weight neonates more often and must be differentiated from HD. Also, MO in very low birth weight neonates should be treated with special attention due to more a complicated clinical course.
Biliary atresia (BA) is an infantile cholestatic disease of progressive obliterative cholangiopathy with varying degrees of damage to both extra and intrahepatic bile ducts due to unknown causes. The diagnostic studies should be done to diagnose or exclude BA without unnecessary delay. Kasai portoenterostomy is the first choice of treatment for bile drainage from microscopic bile ductules present in the portal fibrous mass. The medical management after Kasai portoenterostomy should be done carefully to maintain bile excretion and prevent and treat complications including cholangitis, hepatic fibrosis, portal hypertension and nutritional problem. The reported five years-survival rates after Kasai portoenterostomy range from 30 to 60%. About 20% of all patients undergoing Kasai portoenterostomy during infancy survive into adulthood with their native liver. Even if Kasai portoenterostomy remains as the first line of treatment in BA, liver transplantation serves as a good salvage treatment when portoenterostomy fails or liver function gradually deteriorates after initially successful establishment of bile flow. Overall 5-year survival rate in BA is about 90% in recent series.
Foreign body ingestion is a frequent event in the pediatric age group, but the incidence of foreign bodies in the appendix is very low. The authors report a case of ingested foreign body trapped in the appendix in a 7-year-old girl. The foreign body was successfully treated by laparoscopic appendectomy under fluoroscopic guidance.
The authors applied anterior sagittal transrectal apporach (ASTRA) for the repair of urethrovaginal fistula which developed after total repair of persistent cloaca. The patient had been diagnosed to have persistent cloaca, double uterus and double vagina, and received PSARP, excision of right-side uterus and vagina, and left vaginal switch operation at 22 months old. After operation, the patient admitted several times due to frequent urinary tract infection and ectopic stone formation in bladder and neovagina. Urethro-neovaginal fistula was confirmed by cystoscopy and corrected with ASTRA. Postoperative voiding cystourethrogram showed no fistula tract. ASTRA showed improved surgical field, minimized ureterocystic damage, and preserved perirectal nerve due to limited incision of rectum.
Appendicitis is the most common surgical emergency in childhood and the technologic advances of modern medicine have affected the diagnosis and treatment of appendicitis. This study is to evaluate the differences in diagnosis and treatment of appendicitis between present and 10 year ago. The authors retrospectively reviewed the medical records of patients who underwent appendectomy under the diagnosis of the acute appendicitis from July 1993 to June 1995 (Group A, n = 78) and from July 200 to June 2005 (Group B, n = 105). There are no differences between group A and B in mean age (8.5 ±3.6 vs. 9.3 ±3.1 year), duration of symptoms (3.0 ±3.2 vs. 2.6 ±3.8 days), and postoperative hospital stay(6.6 ±4.8 vs. 5.8 ±3.6 days). Preoperative abdominal ultrasonogram and/or computed tomogram was performed in 7 patients (9.0 %) of group A and in 51 patients (58.5 %) of group B. Thirty-six patients (34.3 %) of group B underwent laparoscopic appendectomy, but none in group A. Incidence of a histologically normal appendix decreased from 15.8 % in group A to 4.8 % in group B (p =0.018). This study suggests that utilization of abdominal ultrasonogram or computed tomogram in preoperative evaluation become more popular and surgical treatment of acute appendicitis become more minimally invasive. The rate of negative appendectomy was also reduced compared with 10 year ago.
Citations

This case report describes a baby who received a laparoscopic gastrostomy tube insertion, which was dislodged accidentally at 16(th) postoperative day. After the dislodgement, cutaneous tract rapidly closed, and reinsertion seemed to be impossible. However, gastrostomy tube was reinserted safely with fluoroscopy-guided Seldinger's technique under local anesthesia with sedation. This is the unique method of modified Seldinger's technique for reinsertion of gastrostomy tube under local anesthesia and sedation for accidentally dislodged gastrostomy tube. This method was thought to be safe, easy and useful technique for gastrostomy reinsertion after dislodgement of gastrostomy tube.
Solid pseudopapillary tumor (SPT) of the pancreas occurs most frequently in the second or third decades of life, and is prevalent in females. Unlike other pancreatic malignancy, SPT usually has a low malignancy potential. This study reviews our clinical experience and surgical treatment of pancreatic SPT. Admission records and follow-up data were analyzed retrospectively for the period between January 1996 and January 2003. Five patients with a pancreatic mass were operated upon and SPT was confirmed by pathology in each case. The male to female ratio was 1 : 4. The median age was 13.8 years. Findings were vague upper abdominal pain (n=5, 100 %) and an abdominal palpable mass (n=3, 60 %). The median tumor diameter was 6.8cm and the locations were 2 in the pancreatic head (40 %) and 3 in the pancreatic tail (60 %). Extra-pancreatic invasion or distant metastasis was not found at the initial operation in all five cases. A pyloruspreserving pancreaticoduodenectomy (n=1) and a mass enucleation (n=1) were performed in two patients of pancreatic head tumors. For three cases of tumors in pancreatic tail, distal pancreatectomy (n=2) and combined distal pancreatectomy and splenectomy (n=1) were performed. The median follow-up period was 60 months(12-117month). During the follow-up period, there was no local recurrence, nor distant metastasis. Postoperative adjuvant chemotherapy or radiotherapy was not carried out. All five children were alive during the follow up period without any evidence of disease relapse. SPT of the pancreas in childhood has good prognosis and surgical resection of the tumor is usually curative.
The prognostic factors for extrahepatic biliary atresia (EHBA) after Kasai portoenterostomy include the patient's age at portoenterostomy (age), size of bile duct in theporta hepatis (size), clearance of jaundice after operation (clearance) and the surgeon's experience. The aim of this study is to examine the most significant prognostic factor of EHBA after Kasai portoenterostomy. This retrospective study was done in 51 cases of EHBA that received Kasai portoenterostomy by one pediatric surgeon. For the statistical analysis, Kaplan-Meier method, Logrank test and Cox regression test were used. A
Citations

Central venous catheter (CVC) for long-term venous access is indispensable for various reasons including hyperalimentation, frequent blood sampling, frequent IV drug use in pediatric patients. We report clinical experience of surgical neonates in whom CVC was inserted primarily via great saphenous vein into suprarenal inferior vena cava. From March 2004 to March 2006, we performed CVC insertion via saphenous vein - contralateral side to main wound - into suprarenal inferior vena cava in surgeries of neonates. 2.7Fr or 4.2Fr, single lumen, tunneled Broviac catheters (Bard Access system, Inc, Salt Lake City, Utah) were used. Skin exit site of tunneled catheter was located in ipsilateral flank area just below edge lower rib. At the end of the procedure, location of the catheter tip was confirmed by plain radiography of abdomen. We retrospectively reviewed the admission records of the patients including nursing staff charts. Nine (50.0 %) patients were male and nine (50.0%) were female. Median gestational age was 38 weeks (range, 29–42 weeks) and median birth weight was 3,105 gm (range, 1,040–3,720 gm). Median age at catheter insertion was 38.5 days (range, 1–236 days). The purpose of CVC insertion was short-and long-term hyperalimentation in nine (50.0 %) patients. CVC insertion was performed in operation room under general anesthesia in sixteen (88.9 %) patients (in these cases, CVC insertion was performed just prior to concurrent operation) and neonatal intensive care unit (NICU) under local anesthesia with adequate sedation in two (11.2%). During the admission period (total catheter-indwelling time : 553 days), CVC functioned well without any significant side effects. Transient swelling of the ipsilateral leg (n=1, 5.6 %) and transient migration of catheter tip (n=1, 5.6 %) were noted, which did not affect function of the indwelled CVC. Mean catheter-indwelling time was 30.7days (range, 3–72 days). All catheters were removed electively except two mortality case. Complications, such as thrombosis, infection, kinking or extravasation of drugs, were not observed in our study period. Tunneled trans-great saphenous vein inferior vena cava catheters are not only comparable to cervical CVCs in terms of function and complication rates, but also very beneficial in selected patients, especially those in whom cervical approach is technically impossible or contraindicated.
Inguinal hernia is the most common disease treated by the pediatric surgeon. There are several controversial aspects of management 1)the optimal timing of surgical repair, especially for preterm babies, 2)contralateral groin exploration during repair of a clinically unilateral hernia, 3)use of laparoscope in contralateral groin exploration, 4)timing of surgical repair of cord hydrocele, 5)perioperative pain control, 6)perioperative management of anemia. In this survey, we attempted to determine the approach of members of KAPS to these aspects of hernia treatment. A questionnaire by e-mail or FAX was sent to all members. The content of the questionnaire were adapted from the “
Citations

Artificial classification of anorectal malformation (ARM) is difficult because it is a spectrum of embryologic maldevelopment. However, the establishment of an ideal classification of ARM should be established in order to choose the adequate treatment and evaluate the prognosis. The classification system of ARM has followed the development of medicine, and the pediatric surgeons, who manage the ARM, should understand the change of this classification system.
Esophageal atresia without tracheoesophageal fistula accounts for 7-11% of all types of esophageal atresia and is very difficult to treat. In our hospital from 1990 to 2005, we operated upon 40 patients with esophageal atresia, and 6 had pure atresia. The preoperative characteristics, operative findings and post operative course of the six patients with pure atresia were analysed. Immediate gastrostomy was performed in all 6 patients. One patient had simultaneous cervical esophagostomy. Esophageal reconstruction procedures were transhiatal gastric pull up in 3 patients, esophagocologastrostomy utilizing left colon in 1, and transthoracic esophagoseophagostomy with esophageal bougination in 2. Postoperative complications were pneumonia, anastomosis leakage, and gastroesophageal reflux symptom. Conservative management was effective in all patients. A larger series of cases would be required to demonstrate the most effective treatment for this particular anomalous condition.
Citations

Recently, the incidence of perinatally detected asymptomatic adrenal gland masses has increased because of widespread use of radiological diagnostic tools. However, optimal treatment of these masses has not been determined. The aim of this study is to elucidate the treatment guideline of perinatally diagnosed adrenal gland masses. The authors retrospectively reviewed the medical records of the 11 patients with asymptomatic adrenal gland mass, detected perinatally, between 1999 and 2004. Six cases were detected by prenatal ultrasound and 5 cases were incidentally detected by postnatal ultrasound. Six patients (surgery group) underwent mass excision. The pathologic diagnoses were neuroblastoma (n=4), adrenocortical adenoma (n=1) and adrenal pseudocyst (n=1). The indications for operation were suspicion of neuroblastoma (n=5) or absence of size decrease during observation (n=1). Three of the 5 suspicious cases of neuroblastoma and one case under observation were proven to be neuroblastoma. There was no surgical complication in the urgery group. All neuroblastoma patients have been well during the follow up period (24.4±14.4 month) without evidence of recurrence. Five cases (observation group) were closely observed because of the benign possibility or size decrease in follow up ultrasound. During the observation period (39±21 week), 4 cases showed complete spontaneous resolution and 1 case showed markedly decreased size of the mass but could not be followed up completely. Surgical resection of the perinatally diagnosed asymptomatic adrenal gland mass is a safe treatment method especially in case of suspicion of neuroblastoma, but closed observation can be applied.
This is a case of tracheomalacia associated with esophageal atresia. An 11-month-old- male boy presented with a life-threatening apneic spell after correction of esophageal atresia (Gross type C). After complete exclusion of the other possible causes of the apneic spell, the presumptive diagnosis of tracheomalacia was made with fluoroscopy and 3-dimensional chest CT. The final diagnosis was made with rigid bronchoscopy under spontaneous respiration. The aortopexy was performed with intraoperative bronchoscopic examination. The postoperative period was unremarkably uneventful. The patient was discharged 9 days after the aortopexy and has remained well to date (5 months after the aortopexy).
Citations

It has been widely accepted that complete surgical resection of hepatoblastoma is essential for long-term survival. But unfortunately less that 50% of hepatic tumors in children can be totally removed at the time of diagnosis. This report is to present the experience of successful resection of hepatoblastoma after concurrent radiotherapy with transarterial chemoinfusion in a child. We believe this modality of treatment enables complete resection of unresectable hepatoblastoma, which is resistant to the systemic chemotherapy.
Slide tracheoplasty, as a treatment for congenital tracheal stenosis, has been recently reported to have good results and quite a number of advantages as compared with conventional tracheoplasties. The aim of this study is to report a new surgical technique modified from the slide tracheoplasty, “the slide cricotracheoplasty” for the congenital cricotracheal stenosis. A girl was born by Cesarean section and the diagnosis of esophageal atresia (Gross type C) and cricotracheal stenosis (30% of total length of trachea) was established. Esophageal atresia was successfully corrected at the 8th day of life. At the 31st day of life, corrective surgery for congenital cricotracheal stenosis, the slide cricotracheoplasty, was performed with success. Slide cricotracheoplasty is almost the same procedure as slide tracheoplasty except for two technical features. First the cricoid cartilage was split on its anterior surface. Second the split cricoid cartilage was fixed to pre vertebral fascia to maintain enough space to accommodate the sliding caudal segment of trachea because of the stiffness of the cricoid cartilage. We believe that the sliding cricotracheoplasty is a new surgical technique for congenital cricotracheal stenosis that has similar results and advantages as the sliding tracheoplasty.
In hepatoblastoma, encouraging cure rates have been achieved with recent advances in chemotherapy and surgical techniques. The aim of this study is to evaluate the role of combined therapeutic modalities and surgical resection in hepatoblastoma. Fifteen cases of hepatoblastoma were treated from January 1993 to August 2000. Six patients had resectable tumors at initial diagnosis. All underwent surgical resection and in four patients postoperative adjuvant chemotherapy was needed. Nine out of 15 patients had unresectbale tumors at initial diagnosis, and preoperative chemotherapy was applied. There was one operative mortality and 14 patients showed good prognosis after surgery. Although various treatment modalities should be combined for the unresectable hepatoblastoma, surgical resection remains the major curative procedure.
Neuroblastoma arises from the embryonic tissue of the adrenergic rest. It is commonly found in children and mostly in nonrenal tissue. We present a case of intrarenal neuroblastoma which was initially thought to be a Wilms' tumor. The patient was a 18 months-old girl treated with radical nephrectomy and adjuvant chemotherapy after operation. The neoplasm within the kidney in children cannot always indicate Wilms' tumor. Neuroblastoma of the adrenal gland or retroperitoneal tissue may often compress or invade the kidney directly or arise from the kidney. Clinical aspects that differentiate between neuroblastoma and Wilms' tumor are discussed with a review of the literatures.
Pseudoaneurysm of splenic artery may arise from a vascular erosion by the inflammatory processes around the splenic artery, particularly in acute pancreatitis and chronic pancreatitis, which may cause rupture of pseudoaneurysm and life threatening hemorrhage. Collective experience with this massive hemorrhage is attended by a high mortality rate even with prompt therapy, and conservative management is associated with an almost 100 per cent of mortality rate. Identification of the bleeding site at laparotomy may be exceedingly difficult, which makes the preoperative detection of bleeding source desirable. Peripancreatic vascular lesions can be identified by angiography, and in selected cases the risk of urgent operation to control massive hemorrhage may be obviated by embolization. The authors have recently experienced a case of ruptured splenic artery pseudoaneurysm combined with a pancreatic pseudocyst in a 6 years old boy. A bolus enhanced CT scan and angiography were essential to confirm these complications of pancreatic pseudocyst. We managed this child successfully with an urgent procedure of transcatheter arterial embolization and another elective surgery of pancreatic pseudocyst.
Femoral hernias are very uncommon in children and very easily misdiagnosed. During a period of three years, three children of femoral hernia were treated by one pediatric surgeon at Severance Hospital. Only one case was diagnosed correctly before surgery; the other two were thought to be either an indirect inguinal hernia or groin mass. Only one patient had curative hernioplasty (McVay hernioplasty) at the first operation; the other two did not have curative hernioplasty at the first operation. Femoral hernia in childhood is a challenging clinical problem because of its rarity and similar clinical presentation as indirect inguinal hernia. The frequency with which an incidental indirect inguinal hernia sac or patent processus vaginalis can be found at surgery can perpetuate a misdiagnosis. The absence of an expected indirect inguinal hernia sac or an apparent recurrence of an indirect inguinal hernia should lead to consideration of possible femoral hernia.
Evaluation of the sacrum in anorectal malformations (ARMs) is important because of the frequent association with ARMs and functional outcome after correction of ARMs. Sacral defects are not easily detected because of immaturity of sacrum in children and overlooking of pediatric surgeons. The authors utilized the sacral ratio in normal children and patients with ARMs. In normal children, the mean true sacral ratio and mean sacrococcygeal ratio were 0.60±0.08 and 0.72±0.13 respectively. Sacral ratio was not correlated with age and did not changed with age in same patient. However, true sacral ratio and sacrococcygeal ratio were significantly lower in patients with high type ARMs than those of normal children (p<0.001). There was no difference between patients with low type ARMs and normal children. These results suggest that abnormal sacrums are more frequently encountered in patients with high type ARMs than in normal children, and that true sacral ratio and sacrococcygeal ratio can be used in the evaluation of the abnormal sacrum.
Citations

Segmental dilatation of small intestine is a rare form of the congenital intestinal anomaly. Many other congenital anomalies have been reported in these patients, but to our knowledge, the association with colonic duplication has not been reported in literatures. We report a case of segmental dilatation of distal ileum associated with colonic duplication. The main clinical and pathogenic aspects are discussed, and the literatures were reviewed.
The anomalous pancreaticobiliary duct union (APBDU) might cause the formation of choledochal cyst and malignancies of hepatopancreaticobiliary system. The purpose of this study is to make an experimental animal model of APBDU similar to that of human. One to two-month-old Mongrel dogs (n=12) were divided into two groups; the control group (n=2) had a sham operation performed, and in the experimental group (n= 10) the end of distal' common bile duct (CBD) was anastomosed to the side of the dorsal pancreatic duct making APBDD. Serum was obtained for chemical analysis on the 10th postoperative day. The dogs were sacrificed at the 5th week (n=3), the 6th week (n=3), the 7th week (n=2), the 8th week (n=2) and the 6th month (n=2) after the experimental surgery. With sacrifice, operative cholangiogram was taken, and bile juice was obtained for chemistry and bacterial culture. The en-bloc specimens of the hepatopancreaticobiliary system were removed for microscopic examination. Serum and bile juice amylase levels were elevated in the experimental group (n=10), but not in the control group (n=2). Operative cholangiograms of control group revealed no evidence of bile duct dilatation.. On the other hand, the bile duct in the experimental group was markedly dilated without any evidence of stenosis at the anastomosis site (n=10). Histologic examination of the hepatopancreaticobiliary system in the experimental group resembled the findings of choledochal cyst in human. The APBDU of this animal model can produce bile duct dilatation by pancreaticobiliary reflux. We think that this animal model can be potentially promising for the research about the APBDU associated hepatopancreaticobiliary diseases.
Citations

We have treated a case of pseudocyst of transverse mesocolon in 3-year-old male child. Operative findings demonstrated that the pseudocyst originated in the transverse mesocolon, and was not connected to the pancreas. A colonic duplication was found incidentally near the pseudocyst. On microscopic examination, ectopic pancreatic tissue was noted in the transverse mesocolon. This pseudocyst was thought to have originated from the ectopic pancreas of the transverse mesocolon. This is the first reported case of pseudocyst originated from ectopic pancreas of the transverse mesocolon, combined with a colonic duplication. The pathogenesis is discussed.
Three cases of laparoscopic splenectomy for hereditary spherocytosis are reported. The average operation time was 100 minutes. This was longer than traditional open splenectomy for the same entity( 63 minutes). Average hospitalization period was 3 days. This was shorter than the hospitalization period for the traditional group(6.2 days).
Transhiatal gastric transpositions were performed in two case of long gap esophageal atresia without tracheoesophageal fistula. The patients were a 12 months old female and an 18 months old male. Stamm type gastrostomies were performed at other hospitals in both cases. The stomach was mobilized preserving the right gastric artery, the right gastroepiploic artery and spleen. The proximal and distal esophageal pouches were excised by transcervical and transhiatal route, respectively. The mobilized stomach was pulled up to the neck through esophageal hiatus and posterior mediastinal route. The esophagogastrostomy, the only one anastomosis of this procedure, was performed in the neck. There was no clinical evidence of anastomotic leakage, stricture, regurgitation, difficulty of gastric emptying, hoarseness or respiratory problem. Transhiatal gastric transposition seems to be a safe and easy alternative surgical procedure for esophageal replacement in long gap esophageal atresia.
Bacillus Calmette-Guerin(BCG) lymphadenitis is a complication of post-BCG vaccination and its treatment is still controversial. Eighty patients who had been operated for BCG lymphadenitis from 1987 to 1996 were reviewed. Thirty-one of them were treated with antituberculous drugs(mean dunition: 3 months) preoperatively and 49 patients were not given preoperative antituberculous medication. No one was treated with antituberculous drugs postoperatively. Operation methods were excision(72) and partial excision with curettage(8). There was no statistical difference in recurrence rate between groups In two patients(2.5 %) treated with preoperative antituberculous drugs, the lesions recurred after operation. The results suggest that preoperative antituberculous medication does not play any role in the treatment of BCG lymphadenitis and in preventing recurrence in surgically excised cases.
Citations

The association of pyloric atresia and epidermolysis bullosa(EB) in newborn is rare and inheritant as an autosomal recessive trait. We report a newborn girl with pyloric atresia and epidermolysis bullosa. Blisters were noted on her skin at birth, especially in pressure-exposed area, and later on the oral mucosa. Junctional epidermolysis bullosa was confirmed by light microscopy and electron microscopy. Radiography revealed pyloric atresia. Segmental resection of 1.5 cm and gastroduodenostomy were carried out at 4 days of age. Protein loosing enteropathy developed after oral feeding. The frequency of episodes of nonscarred blisters and the severity and duration improved significantly with time. The protein loosing enteropathy was persistent, and at 1 year of age, her growth is markedly retarded.
Hyperimmunoglobulin E syndrome is a relatively rare primary immunodeficiency syndrome characterized by recurrent infection, abscess formation and marked elevation of serum IgE level. The common infectious organism is Staphylococcus aureus and recurrent infection indicates some defects in the immunologic system. Although the infection can affect various organs, gastrointestinal tract involvement is rare and only one case of colon perforation has been previously reported. Herein we report another one case of colon perforation which ocurred in an 8-year-old girl with hyperimmunoglobulin E syndrome. The patient was admitted to the hospital due to an abscess on right neck. The diagnosis of hyperimmunoglobulin E syndrome was made because she had eczematoid dermatitis on the face, pneumatocele on left upper lung field and markedly elevated serum Ig E level(> 15,000 IV/ml) with a past histories of frequent scalp abscesses and otitis media. Abdominal pain developed on the 13th day of admission and abdominal plain X-ray revealed free air. An exploratory laparatomy was performed and two free perforations of the transverse colon were noted. Segmental resection and double barrel colostomy were performed. Colostomy closure was done 4 month later and she had no gastrointestinal problem during a follow up period of 15 months.
Percutaneous infraclavicular subclavian catheterization has been widely used for a total parenteral nutrition, hemodynamic monitoring and for venous access in difficult clinical situations. Many authors have claimed the infraclavicular cannulation of the subclavian vein in the tiniest infants can be performed with safety and ease, but there are always possibility of serious complications in this method. We present our experiences of peripheral venous cutdown with Broviac catheter. Author routinely introduced Broviac catheter into central vein via peripheral venous cutdown. There was no life threatening complications and no catheter related death. The complication rate was very low. The catheter related sepsis was documented in only two patient(4.7%). The average catheter longivity was 19.59 days. In view of the safety and low rate of complication, we think that peripheral venous cutdown with Broviac catheter should be the method of choice when central venous access is neccesary in infants. The infraclavicular subclavian catheterization should be reserved in infants with few accessable peripheral vein.