Although nonoperative treatment of appendicitis (NOTA) in the pediatric population has been well reported recently, patient selection and treatment scheme varies among studies, making it difficult to establish treatment standards for NOTA.
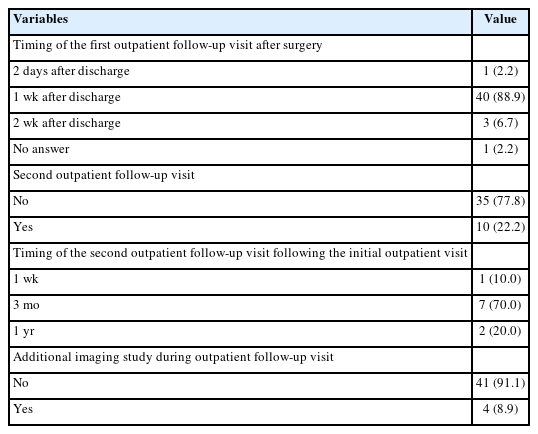
In a single medical center, patients younger than 18 years who were diagnosed with appendicitis: 1) with abdominal pain not exceeding 24 hours, 2) without radiologic evidence of appendicolith or appendiceal perforation or pelvic abscess, and 3) without signs of frank generalized peritonitis were offered NOTA, and their data were prospectively collected.
Twenty-two patients with uncomplicated appendicitis agreed to NOTA and were enrolled in the study. The initial success rate (resolution of abdominal pain and hospital discharge without appendectomy) was 100% (22 out of 22 patients). At a median follow-up period of 23.8 months, two patients had recurrence at two and three months after completion of NOTA. These patients underwent laparoscopic appendectomy.
Stringent patient selection may be necessary to apply NOTA safely for all children with uncomplicated appendicitis. Further studies concerning patient selection and conformed treatment protocols for NOTA are required.
We describe our experience in managing congenital diaphragmatic hernia (CDH) in neonates.
From February 1995 to July 2014, 64 neonates diagnosed with CDH were managed. The medical records of these neonates were retrospectively reviewed.
There were 40 males and 24 females. CDH was on the left side in 44 cases (68.8%), on the right side in 19 cases (29.7%) and bilateral in 1 case (1.6%). Forty-six patients (71.9%) received surgical repair of the hernia while 18 patients (28.1%) died prior to surgery. The timing of surgery was mean 7.0 days after birth. Extracorporeal membrane oxygenation was used in six patients (9.4%), High-frequency oscillation ventilation was used in 49 patients (76.6%), and nitric oxide was used in 42 patients (65.6%). Thirty-three cases (71.7%) of CDH repair were done via open laparotomy, 3 cases (6.6%) by open thoracotomy. and minimally invasive thoracoscopic repair was done in 10 cases (21.7%). Ten cases (21.8%) required patch repair of the CDH. Barotrauma and pneumothorax of the contralateral lung was seen in 16 cases, leading to death in 15 of these cases. The overall survival rate was 48.4% (31/64) and postoperative survival rate was 67.4% (31/46). When all patients are divided into 3 groups by era and analyzed by logistic regression models, the mortality outcome of recent era (2009–2014) was significantly better than that of intermediate era (2002–2008) (29% vs. 71%, p=0.006) and tended to be better than that of past era (1995–2001) (42% vs. 71%, p=0.062).
The overall survival of neonates with CDH at our center has improved over the last two decades. Sixty-four neonates with CDH were managed at a single center and their overall survival was 48.4%. The risk factors for mortality include the occurrence of pneumothorax and right side lesions.
Citations

Hepatocellular carcinoma (HCC) is a rarely occurring disease in the pediatric population. We report our center's experience of management of HCC in children and adolescents.
From 1996 to 2012, 16 patients aged 18 or younger were diagnosed with HCC at our center. The medical records of these 16 patients were retrospectively reviewed.
There were 9 boys and 7 girls. Median age at diagnosis of HCC was 14.5 years. All patient had pathologically confirmed diagnosis of HCC. Three patients had distant metastasis at the time of HCC diagnosis. Eight patients were surgically managed, including 4 liver resections, 3 liver transplantations, and 1 intraoperative radiofrequency ablation. The remaining 8 patients received systemic chemotherapy. Overall, 6 patients are alive at median 63.6 months after diagnosis of HCC. All survivors were surgically managed patients.
HCC is a rare disease occurring in childhood. Patients with systemic disease have poor outcome. Liver transplantation may be a good option for treatment of pediatric HCC.
The congenital H-type rectovestibular fistula, a fistula between the anorectum and genital tract besides a normal anus is a rare variant of anorectal deformities. This disease needs proper treatment but there are no standard of diagnosis and treatment. The purpose of this report is to review a 13-year experience of approach and management for H-type rectovestibular fistula at a single institution.
From February 2002 to August 2015, we cared for 11 patients who had congenital H-type rectovestibular fistula and reviewed their clinical presentation, accompanied anomalies, diagnostic modalities, operative technique, and postoperative progress.
Most patients with H-type rectovestibular fistula presented with symptoms including vestibular defecation and major labial abscess. We could find the fistula tract in most of patients by fistulography using contrast dye. All of the patients had been operated. There were 2 recurrences after surgical treatment who had inflammation and infection associated with the fistula. All other patients recovered without complications.
We think the operation including fistulectomy and repair of perineal body through a transanal approach can be a feasible option to the congenital H-type rectovestibular fistula. Also, combined inflammation and infection should be treated prior to surgery to reduce postoperative complications.
Cervical lymphangiomas are rare lymphovascular malformations arising in the neck, which form huge fluid-containing cysts. Treatment of the malformation consists of surgery and sclerotherapy. However, the optimal approach is still controversial. Here, we describe a series of cervical lymphangiomas which have been treated with surgical approaches.
We retrospectively investigated the medical records of 82 patients who had been diagnosed with cervicofacial lymphangioma from 2001 to 2012 in our center. A closed suction drainage with negative pressure was placed on the operative lesion following excision to prevent reaccumulation of lymphatic fluid and the drainage tube was removed after injecting OK-432 through the tube.
Twelve patients underwent surgical excision of cervical lymphangioma. The median patient age was 3 months at the time of the operation. The patients have been followed-up over a period of 34 months. When lesions were located near vital organs such as the trachea or carotid artery or did not respond to repetitive OK-432 injections, surgical treatment might bring good outcomes. However, swallowing difficulty, lip palsy, or dyslalia due to adjacent nerve damage temporarily appeared as postoperative complications. Five children had tracheostomy due to tracheal or subglottic stenosis and 2 patients had gastrostomy due to aspiration while they eat after surgery.
Surgery for cervicofacial lymphangioma should be conducted carefully in selective cases. A well thought-out surgical plan with a multidisciplinary surgical team approach and placement of closed suction drainage tube after surgery and adjuvant OK-432 sclerotherapy through drainage tube seem to be helpful for good outcome.
Citations

Pediatric liver transplantation has evolved into a definite and effective therapeutic modality for various liver diseases in the pediatric patient. During the last 25 years, liver transplant outcomes in Korea have reached international standards and Korea has become the leader in living-donor liver transplantation. This review will present the cumulative outcomes of pediatric liver transplantation performed in Korea and will focus on other issues of interest involving pediatric liver transplant recipients, especially in the field of immunosuppression and post-transplant lymphoproliferative disease.
Citations