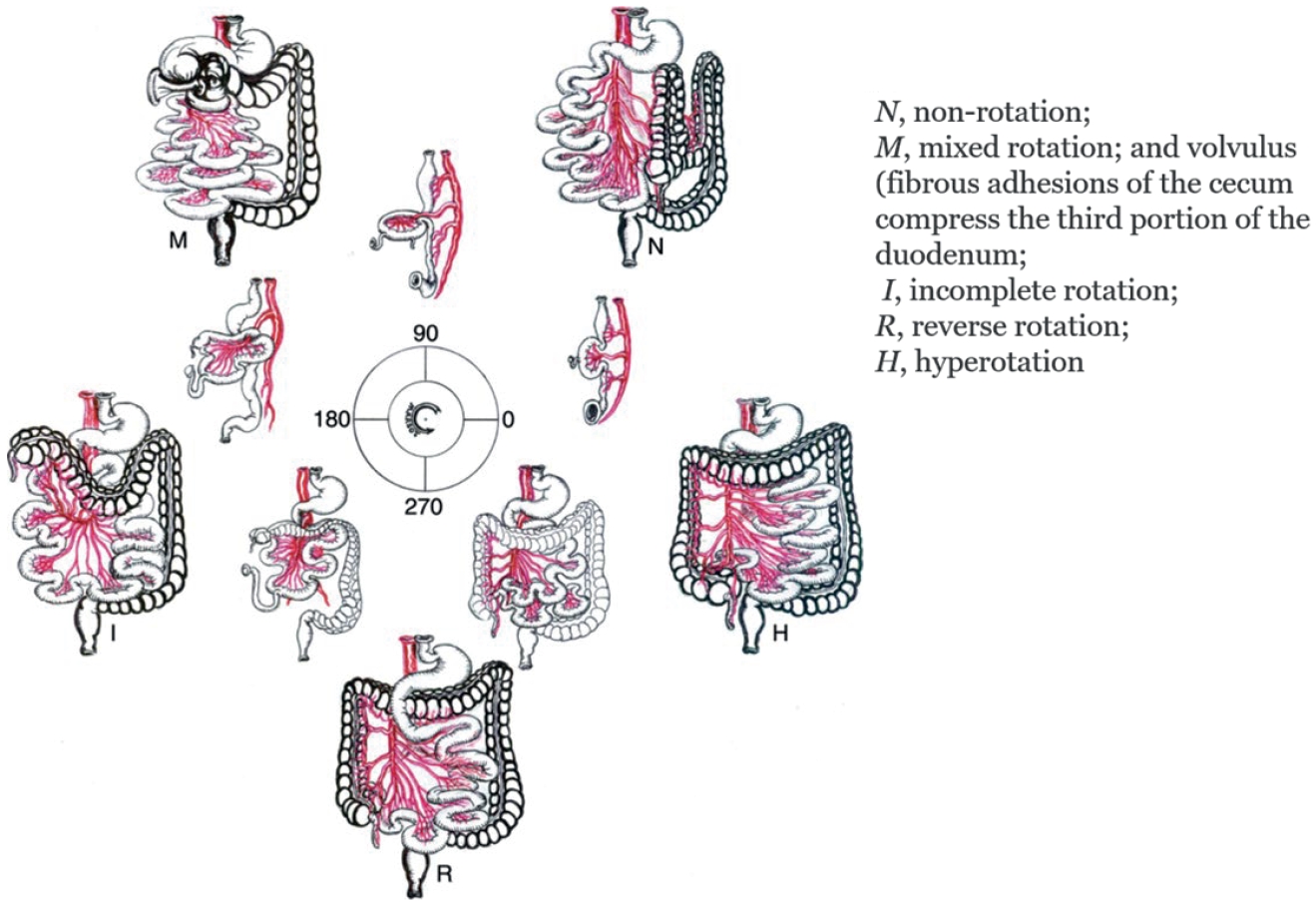
Malrotation is a congenital anomaly that becomes symptomatic more frequently during infancy. The indication for surgical treatment at that age is straightforward. In older children, the diagnosis may be more difficult because of chronic and vague complaint. The aim of this study is to compare the symptoms, rate of volvulus and surgical findings in children younger and older than one year. A retrospective study of 40 patients in a a single medical center diagnosed with malrotation from April 1996 to May 2010 was performed. There were 20 (50%) boys and 20 (50%) girls. At the time of operation, 27 (67.5%) patients were younger and 13 (32.5%) were older than 1 year. Vomiting was seen in 20 cases (74.1%) of the younger group compared to 2 cases (15.4%) of the older group. Abdominal sonography and upper gastrointestinal series showed a sensitivity of 100%. Operative findings: 12 (44.4%) of the younger group presented with volvulus compared to none of the older group. The Ladd's procedure was routinely performed with appendectomy in all cases and bowel resection was requires when volvulus included bowel necrosis or other anomalies were found. After definite procedures, surgical correction for adhesive obstruction was necessary in 5 menbers (18.5%) of the younger group and 1 patient (7.7%) in the older group. There was 1 death due to respiratory failure and pneumonia. Abdominal pain was more frequent symptom and bilious vomiting was less frequent. Volvulus did not occur in the older group. Malrotation should be diagnosed promptly in children over 1 year of age by upper gastrointestinal series and abdominal ultrasonography even though symptoms are not as clear cut as in infants.
Citations

Contralateral groin exploration (CGE) in children with unilateral inguinal hernia remains controversial. Between January 2002 and December 2007, 1967 pediatric patients with inguinal hernia were treated by two surgeons with different criteria of CGE (group A; boys younger than 2 years, older boys prematurely delivered, and all girls, B; birth weight lower than 2kg with inguinal hernia presentation within 6 months after birth, and suspicious physical findings) at Samsung medical center. Patient's age, sex, body weight, diagnosis, and metachronous contralateral inguinal hernia (MIH) incidence were analyzed retrospectively. Among 895 patients in group A, CGE was performed in 460 patients (66.4%) and MIH incidence was 1.7%. In group B, 31 patients (3.5%) had CGE among 1072 patients, and MIH incidence was 4.2%. The average hospital costs of group A and B were 763,956 won and 500,708 won, respectively. The CGE criteria of group B had advantage in total hospital cost. The primary site and the age at presentation had a signiticant effect on the incidence of MIH. But MIH incidence was low and the more contralateral explorations lead to increase of total costs. Therefore, routine contralateral groin exploration and surgery for a patent processus vaginalis could not be justified.
Citations

Peritoneal dialysis (PD) has been utilized for the children with end stage renal disease. Nevertheless, it is thought to promote inguinal hernia by increasing intraabdominal pressure. To investigate the clinical characteristics of inguinal hernia in children on PD, 155 cases of PD in children between January 1996 and June 2007 at Seoul National University Children's Hospital were reviewed retrospectively. Inguinal hernia developed in 16 cases (10.3%, M:F=8:8). Hernia occurrence was not correlated to age. Eleven cases (69%) of inguinal hernia developed in first 6 months after initiation of PD. All inguinal hernias were surgically repaired. No complications occurred related to inguinal hernia or surgery. Recurrent hernia developed in 1 patient (6.3%) of 2 cases who had PD postoperatively on the day of surgery.
In conclusion, inguinal hernia developed more frequently with children on PD than general population (3.5~5%). The rate of hernia development was highest within the first 6 months following initiation of PD. After repair of hernia, we recommend to discontinue PD immediate postoperatively to prevent recurrence.
Pediatric lymphangioma can occur at any site. However the neck is the most common site. There are two treatment modalities (surgical excision and intralesional injection) for lymphangiomas. But, the treatment guide line for lymphangioma has not been established, yet. The aim of this study is to establish the treatment guide line based on our experience with lymphangiomas. Medical records of 82 cases of lymphangioma were reviewed retrospectively. On MRI (magnetic resonance image) findings, lymphangiomas were divided into 4 groups by the proportion of the cyst bigger than 2 cm in diameter of the tumor; group A-proportion of cyst occupies more than 75 %, group B-proportion of the cyst 50~75 %, group C-25~50 %, and D in less than 25 %. All patients were treated with OK-432 intralesional injection as the initial treatment. The effective response rates of OK-432 in group A & B were 88.2 % and 88.8 %, respectively. Group C response was 38.0 % and D only 20.0 %. Twenty-three patients received surgical excision. The result of surgical excision was generally satisfactory. Surgical site infection occurred in 1 case and postoperative bleeding in 1 case. Theses results indicate that intralesional injection of OK-432 could be the first line therapy in group A & B. In group C, OK-432 would be better as the first line therapy than surgery. For the group D, surgical excision should be the first line of treatment.
Citations

Catheter related and perianal problems are common surgical complications encountered during the treatment of pediatric malignancies. However acute surgical abdominal emergencies are rare. The aim of this study is to review acute surgical abdominal complications that occur during the treatment of childhood malignancies. Out of a total of 1,222 patients who were newly diagnosed with malignant disease, between January 2003 and May 2008, there were 10 patients who required surgery because of acute abdominal emergencies. Their medical records were reviewed retrospectively. Hematologic malignancies were present in 7 patients (4 leukemia, 2 lymphoma, 1 Langerhans cell histiocytosis) and solid tumors in 3 patients (1 adrenocortical carcinoma, 1 desmoplastic small round cell tumor, 1 rhabdomyosarcoma). Seven patients had intestinal obstruction, two had gastrointestinal perforation and one, typhlitis. Intestinal obstructions were treated with resection of the involved segment with (N=2) or without (N=3) enterostomy. Two patients had enterostomy alone when resection could not be performed. Intestinal perforation was treated with primary repair. Typhlitis of the ascending colon was treated with ileostomy. Right hemicolectomy was necessary the next day because of the rapidly progressing sepsis. Three patients are now alive on chemotherapy and one patient was lost to followed-up. Among six patients who died, five died of their original disease progression and one of uncontrolled sepsis after intestinal perforation. Although rare, acute surgical abdominal complications can occur in childhood malignancies. Rapid and accurate diagnosis and appropriate operation are required for effective treatment of the complications.
Neuroblastoma is the most common extracranial solid tumor in children, and accompanies various clinical symptoms including hypertension. Hypertension is associated with catecholamines secreted from the tumor, and is usually not severe. We report one case of malignant hypertension with cardiac failure in a patient with adrenal neuroblastoma, successfully treated with adrenalectomy. A 3 year-old boy complained of protrusion of the chest wall. Physical examination revealed severe hypertension with cardiac failure. The levels of metabolites of catecholamine were increased in blood (norepinephrine >2000 pg/mL) and urine (norepinephrine 1350.5 ug/day). Abdominal CT showed a 7 cm-sized solid mass arising from the right adrenal gland. After stabilizing the hemodynamics with oral phenoxybenzamine, right adrenalectomy was performed. Pathological diagnosis was a ganglioneuroblastoma. The hypertension and cardiac failure were resolved after tumor removal.
Splenic cystic lesion is uncommon in children, and cystic lymphangioma of the spleen has not been reported in Korean pediatric patients. Here we report a case of cystic lymphangioma arising from the spleen in a 16 year-old male. The patient presented with left flank pain for 5 days after blunt trauma to the same site. On physical examination, left abdominal tenderness and a palpable spleen were noted. Abdominal ultrasound and MRI revealed multiple septated macro-cystic mass abutting to the spleen medially, suggestive of cystic lymphangioma of the spleen. Laparotomy revealed a 20 cm sized cyst in the spleen, and 2,000mL of dark-brownish fluid was aspirated from the cyst. Splenectomy was performed. Pathological examination revealed the cystic lymphangioma. Post-operative recovery was uneventful, and the patient was discharged at 7 days after surgery.
With the widespread use of the obstetrical ultrasound, identification of a fetal suprarenal mass becomes more common. Most of these masses prove to be congenital neuroblastomas (CNB) postnatally. However, the diagnosis is often confused with other benign lesions and the post-natal management remains controversial. The medical records of 13 patients that underwent primary surgical excision for an antenatally detected adrenal CNB, between January 1995 and April 2009, were reviewed retrospectively. The clinical, radiological, surgical, and pathological data on the suprarenal mass were collected. Staging evaluation was performed after histological confirmation of the CNB. Most of the CNBs were stage I (N=11), with 1 stage IV and 1 stage IV-S. Four patients (3 stage I and 1 stage IV-S) had N-myc gene amplification. The stage I patients were cured by surgery alone, and stage IV patients underwent 9 cycles of adjuvant chemotherapy and currently have no evidence of disease after 39 months of follow-up. The patient with stage IV-S is currently receiving chemotherapy. There were no post-operative complications. For early diagnosis and treatment, surgical excision should be considered as the primary therapy for an adrenal CNB detected before birth. The surgery can be safely performed during the neonatal period and provides a cure in most cases. Surgical diagnosis and treatment of CNB is recommended in neonatal period.
Citations

Neuroblastoma is the most common extracranial solid tumor in children. We retrospectively analyzed the results of neuroblastoma treatment of 191 patients (116 males and 75 females) treated between January 1986 and December 2005 at the Department of Pediatric Surgery and the Department of Pediatrics, Seoul National University Children's Hospital. The mean age at diagnosis was 3.1 years (0.1 yrs - 13.5 yrs). Forty-seven patients were under 1 year of age. The mean follow-up period was 57.3 months (24 days - 19.1 yrs). Patients were classified into two groups according to the completeness of resection of the primary tumor; (1) gross total resection (GTR) and (2) incomplete resection (IR). The number of patients in stages I, II, III, IV, IV-S were 17 (8.9 %), 12 (6.3 %), 43 (22.5 %), 114 (59.7 %), 4 (2.1 %), respectively. GTR was achieved in 120 patients and IR in 71 (22 stage III, 47 stage IV, 1 stage IV-S, 1 brain). Overall survival (OS) was 65.2 % and event-free survival (EFS) was 48.6 %. EFS were 100 %, 75 %, 66.8 %, 31.3 %, 75 % at stage I, II, III, IV, IV-S, respectively. There was no significant difference in EFS according to the completeness of resection. EFS was improved in GTR group (p=ns) of stage III, but by contrast, stage IV patients showed worse EFS in GTR group. EFS was improved significantly after the introduction of autologous stem cell transplantation (ASCT) (58.1% vs. 40.6%, p=.029). The EFS improved significantly after the introduction of ASCT in IR group (p=.009) rather than GTR group (p=ns). The EFS of the patients under 1 year of age (N=47) was better than the patients over 1 year of age (N=144) significantly (75.5 % vs. 39.4 %, p=.0034). The prognosis of neuroblastoma was related to the INSS stage and age at diagnosis. The survival of IR group significantly improved after ASCT.
The survival of Very Low Birth Weight (VLBW) infants has been improved with the advancement of neonatal intensive care. However, the incidence of accompanying gastrointestinal complications such as necrotizing enterocolitis has also been increasing. In intestinal perforation of the newborn, enterostomy with or without intestinal resection is a common practice, but there is no clear indication when to close the enterostomy. To determine the proper timing of enterostomy closure, the medical records of 12 VLBW infants who underwent enterostomy due to intestinal perforation between Jan. 2004 and Jul. 2007 were reviewed retrospectively. Enterostomy was closed when patients were weaned from ventilator, incubator-out and gaining adequate body weight. Pre-operative distal loop contrast radiographs were obtained to confirm the distal passage and complete removal of the contrast media within 24-hours. Until patients reached oral intake, all patients received central-alimentation. The mean gestational age of patients was 26+2 wks (24+1~33+0 wks) and the mean birth weight was 827 g (490~1450 g). The mean age and the mean body weight at the time of enterostomy formation were 15days (6~38 days) and 888 g (590~1870 g). The mean body weight gain was 18 g/day (14~25 g/day) with enterostomy. Enterostomy closure was performed on the average of 90days (30~123 days) after enterostomy formation. The mean age and the mean body weight were 105 days (43~136 days) and 2487 g (2290~2970 g) at the time of enterostomy closure. The mean body weight gain was 22 g/day after enterostomy closure. Major complications were not observed. In conclusion, the growth in VLBW infants having enterostomy was possible while supporting nutrition with central-alimentation and the enterostomy can be closed safely when the patient's body weights is more than 2.3 kg.
Citations

Sialoblastoma is a rare tumor of salivary gland origin, developing in the fetal or neonatal period. Most tumors arise in parotid gland, and rarely in submandibular gland. Because of its rare incidence, diagnosis of the sialoblastoma in head and neck tumors of children is not easy. The case of a congenital submandibular gland sialoblastoma is presented. A neonate was transferred right after birth due to a submandibular mass. CT scan showed a lobulating mass located posterior to the left submandibular gland, suggesting neurogenic tumor or myofibroma. The tumor was excised easily after division of a duct-like structure connecting with the submandibular gland. The microscopic findings showed the basaloid cells and ductules forming cellular nests, separated by thin fibrous tissue. Immunohistochemical staining was positive for cytokeratin, vimentin and Ki-67, which was consistent with sialoblastoma.
Citations

The survival rate for rhabdomyosarcoma (RMS) has significantly improved after the introduction of combined multimodality treatment. We report the 20-year treatment outcome of pediatric rhabdomyosarcoma in a single institution. The medical records of 16 patients treated for rhabdomyosarcoma between December 1986 and August 2007 at the Department of Pediatric Surgery, Seoul National University Children's Hospital, were retrospectively reviewed. Mean age at diagnosis was 7.1 years (range: 1.3-14.2 years). Retroperitoneum was the most common primary site (n=7, 43.8%), and embryonal type was predominant (n=11, 6%). Before the treatment, most patients were in advanced TNM stage (stage III 50%, IV; 25%). The patient distribution according to the Intergroup Rhabdomyosarcoma Study Clinical Grouping System (IRS-CGS) was as follows; Group I 31.3%, Group II 12.5%, Group III 31.3% and Group IV 25%. Patients were classified into three groups according to the extent of resection of the primary tumor; complete resection (CR, n=5; 31.3%), gross total resection (GTR, n=7; 43.8%) and incomplete resection (IR, n=4; 25%). Recurrence was observed in 9 patients (56.3%) while there was no recurrence in CR patients. All patients with recurrence were identified as moderate or high-risk according to the IRS-V Risk Group. Pre-treatment TNM stage of RMS in our institution was advanced with aggressive clinical feature, however post-surgical conditions according to IRS-CGS were similar to the previous reports by IRS. This suggests that down-staging of IRS-CGS was achieved with multimodality treatment with CR or GTR. It also suggests that complete resection is the most important prognostic factor in the treatment of RMS in children. Patients classified as moderate or high-risk need close follow-up due to high recurrence rate. In case of localized recurrence, better outcome may be achieved with multimodality treatment including limited surgery.
Inflammatory myofibroblastic tumor (IMT) is a rare reactive lesion characterized by the feature of myofibroblasts and a mixed inflammatory infiltrate that rarely undergoes malignant transformation. Extrapulmonary IMTs in children have been described involving the mesentery, omentum, retroperitoneum, abdominal soft tissues, liver, bladder, mediastinum, head and neck, extremity, appendix, and kidney. Medical records of children treated with abdominal IMT between 1985 and 2005 were reviewed retrospectively. Seven children were treated for IMT with the mean age of 3y 2m (range, 1y 1m to 14y). Tumors were located in transverse mesocolon (n=2), omentum (n=1), porta hepatis (n=2), complex site (antrum, duodenum, common bile duct, porta hepatis) (n=2). The symptoms included abdominal mass, fever, jaundice, abdominal pain and anemia. The masses were excised totally in transverse mesocolon, omentum IMT and there is no evidence of recurrence (follow-up periods: 6y 8m, 8y 9m, 4y 10m). In porta hepatis IMT, liver transplantations were performed and there is no evidence of recurrence (follow period: 6y 8m, 8y 7m). In one case of complex site IMT, partial excision of mass was performed and he still survived with no change of the residual tumor during follow-up period. The other one of complex site IMT denied further treatment after the biopsy. In conclusion, complete surgical excision including liver transplantation and close follow-up are mandatory for the abdominal IMT in child.
Citations

Infantile hepatic hemangioendothelioma (IHHE) is the most common benign vascular hepatic tumor in children. We analyzed the 17-year experience of IHHE. The medical records of 16 patients (M:F=8:8) treated at the Department of Pediatric Surgery and the Department of Pediatrics Seoul National University Children's Hospital between January 1991 and January 2008 were reviewed retrospectively. Mean age at presentation was 87 days (1 day-551 days). Seventy five percent of patients were diagnosed with imaging study and 25% with biopsy. Major symptoms were hepatomegaly (N=5), palpable abdominal mass (N=4) and congestive heart failure (N=3). Six patients had no symptoms. Kasabach-Merritt syndrome was combined in one patient. Nine patients (56.3%) underwent operation and 2 patients (12.5%) underwent only medical treatment. Clinical observation was tried on 5 patients (31.3%) without any treatment. Operation was performed on the patient with clinical symptoms or on patients where the differentiation between begin and malignant could not be determined. Patients who had clinical symptoms but tumor was unreresectabile were treated medically. Among the 5 patients who had been observed for their clinical course, 2 patients showed complete regression and the tumors of the remaining 3 patients were regressing. Clinical symptoms, the age at presentation, the size of tumor and α-FP, all had no significant statistical relationship with the time required for complete tumor regression. There was no relationship between the size change of the tumor and the change of α-FP level. Only the size of tumor was related with clinical symptoms. One patient died of post-operatvie bleeding. Treatment plan was determined by the extent of the tumor and the presence of clinical symptoms. Observation was enough for the patients without clinical symptoms and complete resection was curative for patients with clinical symptoms. Medical treatment is an alternative for the patient whose tumor is unresectable.
Citations

The usefulness of totally implantable central venous port for long-term intravenous infusion is widely accepted in children. Usually the catheters are placed through the internal or external jugular vein. In case of jugular vein cut-down, two separate incisions are needed for catheter and port respectively. Patients also feel uncomfortable as the catheter run through the neck. However these disadvantages can be overcome by using the cephalic vein (CV). We reviewed our experiences on CV cut-down for totally implantable central venous port in children. From January 2002 to December 2006, 201 patients (M:F=127:74) underwent 218 central venous port insertions. Mean age at operation was 5.9 years (2 months - 19 years). Indications included chemotherapy (N=167), long-term intravenous antibiotics infusion (N=36), and total parenteral nutrition (N=15). CV was selected preferentially. The incision includes the deltopectoral triangle laterally, and both the CV cut-down and port insertion were achieved with a single incision. The number of insertion through external, internal jugular vein, and CV was 77, 66 and 75, respectively. The median age, height and body weight were higher in CV cut-down group. The youngest age for CV cut-down was 8 months, the shortest height was 69 cm and the smallest body weight was 5.9 kg. Of 118 trials of CV cut-down, cut-down was successful in 75 cases (63.6 %). CV was absent in 10 cases(8.4 %) and CV was sacrificed after catheter tip malposition in 10 cases (8.4 %). There was only one complication, in which the catheter was inserted into the minute branch of subclavian artery. The CV cut-down method for totally implantable central venous port was safe and feasible in selected groups of patients in children. In addition, preservation of jugular vein and a more favorable cosmetic effect are other benefits of CV cut-down.
Migration of a peritoneal catheter of a ventriculoperitoneal shunt into the scrotum is a rare complication. We treated a case of catheter migration in the scrotum. A 12-year old boy, who had had a ventriculoperitoneal shunt at the age of 4 months due to neonatal hydrocephalus, visited the outpatient clinic because of a right inguinal hernia. On physical examination, a firm mass was found in the left scrotum. Pelvic X-ray demonstrated a coiled catheter in the left scrotum. The catheter was successfully removed by exploring the left patent processus vaginalis after high ligation of the hernia sac. This case suggests a suction action of the patent processus vaginalis and the possibility of catheter migration long after shunt catheter insertion.
Citations

Adrenocortical tumors are very rare in children and the clinical course is not clearly understood. The aim of this study is to review the clinical characteristics and courses of pediatric adrenocortical tumors. The medical records of patients who underwent surgery for primary adrenal tumor at the Department of Surgery, Seoul National University hospital, from Jan. 1986 to Feb. 2006 were reviewed. There were 10 adrenocortical tumor patients; 5 had adrenocortical adenoma and 5 adrenocortical carcinoma. All of the adrenocortical adenomas presented as functioning tumors,
Citations

We reviewed the records of 25 patients who were re-operated upon after primary repair of esophageal atresia with or without fistula at the Department of Pediatric Surgery, Seoul National University Children's Hospital, from January 1997 to March 2007. Types of the esophageal atresia anomalies were Gross type A in 5 patients, C in 18, and E in 2. The indications for re-operation were anastomosis stricture (n = 14), tracheo-bronchial remnant (n = 4), persistent anastomosis leakage (n = 3), recurrent tracheo-esophageal fistula (n = 2) and esophageal web (n = 2). The interval between primary and secondary surgery was from 48 days to 26 years 5 months (mean: 2 years and 4 months). Four patients required a third operation. The interval between the second and third operation was between 1 year 1 month and 3 year 10 month (mean: 2 years 5 months). Mean follow up period after last operation was 35 months (1 years–8 years 6 months). The secondary surgery was end-to-end esophageal anastomosis in 15, esophagoplasty in 5, gastric tube replacement in 5. After secondary operation, 6 patients had anastomosis stricture (4 patients were relieved of the symptoms by balloon dilatation, 2 patients underwent tertiary operation). Five patients had leakage (sealed on conservative management in all). Two patients had recurrent tracheo-esophagel fistula (1 patient received chemical cauterization and 1 patient underwent tertiary operation). Currently, only one patient has feeding problems. There were no mortalities. Secondary esophageal surgery after primary surgery for esophageal atresia was effective and safe, should be positively considered when complications do not respond to nonoperative therapy.