Neonatal neuroblastoma (NBL) is the most common malignant tumor in neonates, but there have been few studies about it. The purpose of this study was to investigate the clinical features of NBL and to compare prenatal and postnatal diagnosed groups.
Nineteen patients who were diagnosed with NBL prenatally or within 28 days after birth from February 1986 to February 2013 in Seoul National University Hospital were enrolled in the study. The patients were categorized according to the International Neuroblastoma Staging System (INSS) and Children's Oncology Group (COG). Retrospective medical-record reviews were performed on these patients. The operative date, complication, pathological stage, and overall survival of the prenatally diagnosed group and the postpartum diagnosed group were compared.
Tumor was detected via prenatal ultrasonography in 8 patients (42.1%), and 11 patients (57.9%) were diagnosed within 28 days after birth. Based on INSS, the patients were divided into the stage I (n=8), stage II (n=1), stage III (n=3), stage IV (n=4), and stage IVs (n=3) groups, respectively. Based on COG, on the other hand, the patients were divided into the low-risk (n=8), intermediate-risk (n=8), and high-risk (n=3) groups. The postoperative complication rate was 29%. One patient died from complications from chemotherapy. The other 18 patients' mean follow-up period was 77.7 months. The differences between the postoperative complication rate, proportion of early-stage tumor, and overall survival of the prenatal and postnatal groups were not statistically significant (p=0.446, p=0.607, p=0.414).
NBL showed favorable outcomes but relatively higher postoperative complications. There seem to be no significant statistical differences in the postoperative complications, proportion of early-stage tumor, and overall survival between the prenatally diagnosed group and the postpartum diagnosed group.
Neuroblastoma is the most common extracranial solid tumor in children, and accompanies various clinical symptoms including hypertension. Hypertension is associated with catecholamines secreted from the tumor, and is usually not severe. We report one case of malignant hypertension with cardiac failure in a patient with adrenal neuroblastoma, successfully treated with adrenalectomy. A 3 year-old boy complained of protrusion of the chest wall. Physical examination revealed severe hypertension with cardiac failure. The levels of metabolites of catecholamine were increased in blood (norepinephrine >2000 pg/mL) and urine (norepinephrine 1350.5 ug/day). Abdominal CT showed a 7 cm-sized solid mass arising from the right adrenal gland. After stabilizing the hemodynamics with oral phenoxybenzamine, right adrenalectomy was performed. Pathological diagnosis was a ganglioneuroblastoma. The hypertension and cardiac failure were resolved after tumor removal.
With the widespread use of the obstetrical ultrasound, identification of a fetal suprarenal mass becomes more common. Most of these masses prove to be congenital neuroblastomas (CNB) postnatally. However, the diagnosis is often confused with other benign lesions and the post-natal management remains controversial. The medical records of 13 patients that underwent primary surgical excision for an antenatally detected adrenal CNB, between January 1995 and April 2009, were reviewed retrospectively. The clinical, radiological, surgical, and pathological data on the suprarenal mass were collected. Staging evaluation was performed after histological confirmation of the CNB. Most of the CNBs were stage I (N=11), with 1 stage IV and 1 stage IV-S. Four patients (3 stage I and 1 stage IV-S) had N-myc gene amplification. The stage I patients were cured by surgery alone, and stage IV patients underwent 9 cycles of adjuvant chemotherapy and currently have no evidence of disease after 39 months of follow-up. The patient with stage IV-S is currently receiving chemotherapy. There were no post-operative complications. For early diagnosis and treatment, surgical excision should be considered as the primary therapy for an adrenal CNB detected before birth. The surgery can be safely performed during the neonatal period and provides a cure in most cases. Surgical diagnosis and treatment of CNB is recommended in neonatal period.
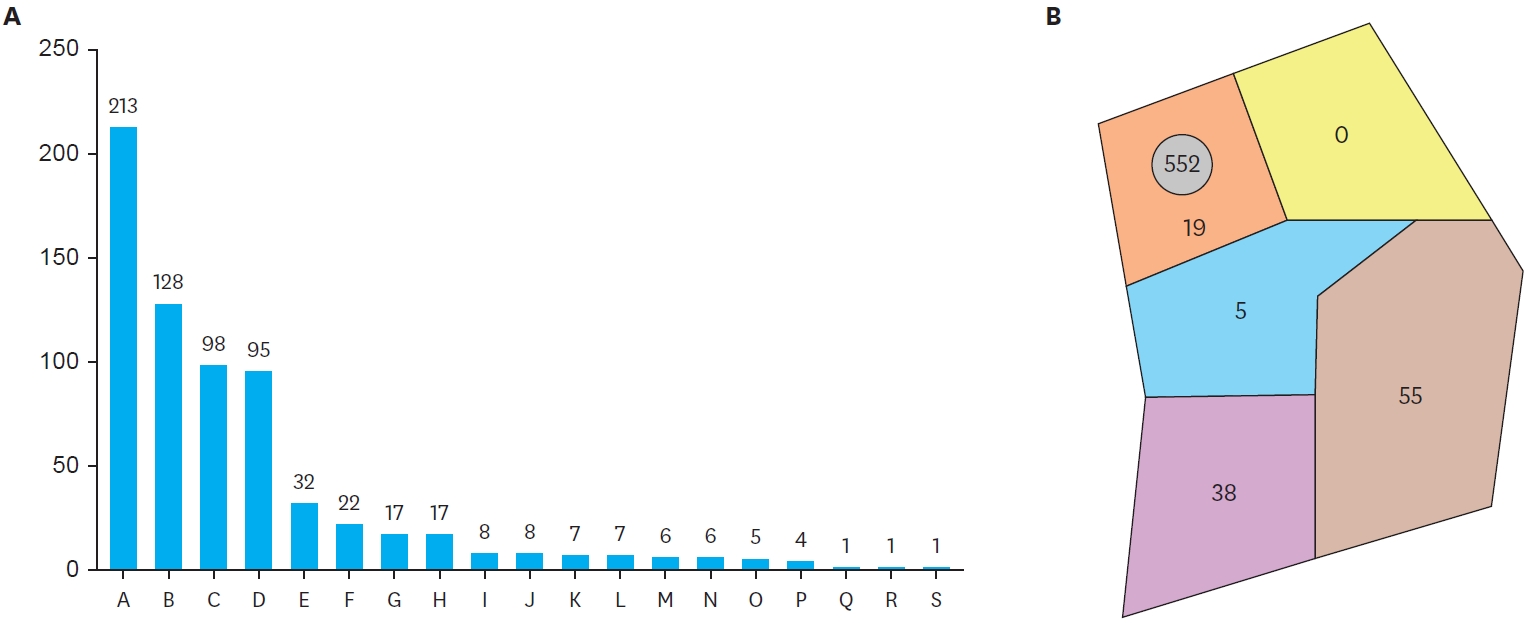
Neuroblastoma is the most common extracranial solid tumor in children. We retrospectively analyzed the results of neuroblastoma treatment of 191 patients (116 males and 75 females) treated between January 1986 and December 2005 at the Department of Pediatric Surgery and the Department of Pediatrics, Seoul National University Children's Hospital. The mean age at diagnosis was 3.1 years (0.1 yrs - 13.5 yrs). Forty-seven patients were under 1 year of age. The mean follow-up period was 57.3 months (24 days - 19.1 yrs). Patients were classified into two groups according to the completeness of resection of the primary tumor; (1) gross total resection (GTR) and (2) incomplete resection (IR). The number of patients in stages I, II, III, IV, IV-S were 17 (8.9 %), 12 (6.3 %), 43 (22.5 %), 114 (59.7 %), 4 (2.1 %), respectively. GTR was achieved in 120 patients and IR in 71 (22 stage III, 47 stage IV, 1 stage IV-S, 1 brain). Overall survival (OS) was 65.2 % and event-free survival (EFS) was 48.6 %. EFS were 100 %, 75 %, 66.8 %, 31.3 %, 75 % at stage I, II, III, IV, IV-S, respectively. There was no significant difference in EFS according to the completeness of resection. EFS was improved in GTR group (p=ns) of stage III, but by contrast, stage IV patients showed worse EFS in GTR group. EFS was improved significantly after the introduction of autologous stem cell transplantation (ASCT) (58.1% vs. 40.6%, p=.029). The EFS improved significantly after the introduction of ASCT in IR group (p=.009) rather than GTR group (p=ns). The EFS of the patients under 1 year of age (N=47) was better than the patients over 1 year of age (N=144) significantly (75.5 % vs. 39.4 %, p=.0034). The prognosis of neuroblastoma was related to the INSS stage and age at diagnosis. The survival of IR group significantly improved after ASCT.
Neuroblastoma arises from the primitive neural crest cells, and is a common malignancy in childhood. The clinical features are characterized by biological heterogeneity. Neuronal degeneration and differentiation occur in some patients. However treatment in the high risk group accounting for approximately half, has not been satisfactory despite a multimodal approach. Therefore, effective treatment is determined by the risk group of prognostic factors, such as age at diagnosis, stage of disease, pathological finding and N-myc amplification. Neuroblastoma can be diagnosed prenatally, which suggests its origin during the normal embryogenesis. Recent knowledge of molecular biology, such as Trk genes, and the concept of cancer stem cells have given us some improved understanding on this disease. Currently, targeted therapies based on the molecular biology of neuroblastoma are under investigation and increasing survival rate and decreasing late complications could be appreciated.
Neuroblastoma treatment remains challenging, but has been advanced by the establishment of clinical and biological variables that determine prognostic risks. Initially, stage and age were the prime determinants of survival used in clinical practice. Risk-based therapy currently is the hallmark of neuroblastoma treatment. This study reviewed the results of neuroblastoma in one center. Sixty-three patients with neuroblastoma were treated primarily at our institution from 1989 to 2003. All patients were graded according to the International Neuroblastoma Staging System (INSS) at diagnosis. There were 37 boys and 26 girls. The median age was 2.14 years (range, 33 days-10.2years). The primary site was the adrenal gland in 47, dumbbell shape extended into spinal canal in 6, retroperitoneum in 5, mediastinum in 3, and other sites in 2. The probability of 5-year overall survival (OS) and event free survival (EFS) were 46.7% and 44.2% by Kaplan-Meier method. According to INSS, there were stage 1 in 2, stage 2 in 5, stage 3 in 12, stage 4 in 42, and stage 4s in 2. There were statistically significant differences in the survival rates between patients with stage1, 2 and stage 3, 4(p<0.05). For the stage 3 and 4, the extent of surgical resection determined from the operative records and pathologic reports assessed extent of surgical resection as complete resection, no visible tumor (CR, n=17); minimal residual, visible tumor less than 5% (MR, n=15); partial resection, more residual tumor than MR (PR, n=11). The 5-year OS rate was 57.8, 51.4, and 13.6% for CR, MR, and PR. There is a trend toward higher OS with achieving the completeness of resection (p<0.05). We conclude that age and stage at diagnosis are prognostic factors, and complete excision of the primary tumor can provide better prognosis for patients with stage 3 and 4 neuroblastoma.
The antiangiogenic effects of novel agent KJ3, Betulinic acid, and Fumagillin on the neovascularization were studied by examining ultrastructural alterations in the vasculature of synthetic gelform and mouse neuroblastoma C1300. Small pieces of gelform with 0.4 % agar were introduced subcutaneously (s.c.) in 7 week old male CH3/HeJ mice. After the LD50s were determined by FACS analysis, a third of LD50 of three drugs were injected either locally or intraperitoneally every other day for 14 days. A/J mice were inoculated s.c. with the C1300 neuroblastoma cell line, then either saline or three drugs were injected in the same manner. The antiangiogenic effects of three drugs were studied by measuring the histologic changes in tumors, and immunostaining for CD34, VIII/vWF, CD105, and thymidine phosphorylase. In the drug treated groups, the number of vessels in gelform experiments and C1300 neuroblastoma experiments were lower than the corresponding values in the control. The histologic findings were significantly different in drug treated groups on day 7, but these were not significant on day 14. These results imply that antiangiogenic agents were effective when the tumor burden is minimal.
Prenatally diagnosed neuroblastomas have been reported in increasing numbers over the past several years. The vast majority are in favorable stages of the disease (stage I, II, IV-S). The authors experienced one case of stage IV-S neuroblastoma of the adrenal gland with liver metastasis, which regressed spontaneously after removal by adrenalectomy. This patient was noticed to have an abdominal mass at prenatal ultrasonography performed at 36weeks of gestation. This tumor was a neuroblastoma of the left adrenal gland with multiple liver metastases. Left adrenalectomy and liver biopsy were performed at 3 months of age. Thirty-eight months after surgery, an MRI demonstrated that the hepatic metastatic lesions had completely regressed without chemotherapy or radiation.
Neuroblastoma arises from the embryonic tissue of the adrenergic rest. It is commonly found in children and mostly in nonrenal tissue. We present a case of intrarenal neuroblastoma which was initially thought to be a Wilms' tumor. The patient was a 18 months-old girl treated with radical nephrectomy and adjuvant chemotherapy after operation. The neoplasm within the kidney in children cannot always indicate Wilms' tumor. Neuroblastoma of the adrenal gland or retroperitoneal tissue may often compress or invade the kidney directly or arise from the kidney. Clinical aspects that differentiate between neuroblastoma and Wilms' tumor are discussed with a review of the literatures.
The WDHA syndrome characterized by watery diarrhea, hypokalemia, and achlorhydria (WDHA syndrome) is rare, and with neurogenic tumors. A 20-month-old girl presenting with symptoms of WDHA syndrome was transferred to our hospital. She had a ganglioneuroblastoma of the adrenal gland. The serum level of VIP was elevated. After complete excision of the tumor, all symptoms related to the WDHA syndrome were relieved and serum VIP level dropped to normal. The postoperative course was uneventful. The patient was treated with postoperative chemotherapy and radiation therapy. There was no evidence of disease 33 months after operation.
Neuroblastoma derived from neural crest cells of the sympathetic nervous system, is the most common extracranial solid tumor in children with many interesting features. It has the highest rate of spontaneous regression, yet has one of the poorest outcome results. Recent updates have shown much increased outcomes in multitreatment approaches and early diagnosis with screening. Authors have studied 42 patients who have been diagnosed and treated in the last decade in the Severance and Yongdong Severance Hospital respectively. They were followed up till January 1998 and was analyzed in terms of age, sexual difference, admission period, staging, diagnostic studies, clinical symptoms and physical examinations, operative time, treatment modalities, survival rate. Twenty eight patients underwent operative procedures, 16 patients had postoperative chemotherapy, and 19 patients had preoperative chemotherapy. Sexual difference was 1.33:1 in favor of males, and 43% of patients were under the age of one year. The patients were initially diagnosed symptomatically, and the abdominal mass was the most common clinical symptom. Eighty six percent of the patients were of advanced stages (>Stage III of INSS), and the 2 year survival rate showed 59.2% and the 5 year survival rate was 29.6%.
Neuroblastoma is the most common solid malignancy in childhood. However, a neuroblastoma presenting as bilateral and multifocal is very rare. A male newborn weighing 2.7 kg was born by normal vaginal delivery at 39 weeks' gestation to a 27-year-old mother who had a normal pregnancy. He was in good condition at birth but presented palpable masses in the both upper abdomen and both side of the neck. Ultrasound examination showed the lesions to be 3 × 3cm sized calcified mass in right suprarenal area and 5 × 3cm sized homogenous mass in left suprarenal area. The abdominal mass was also examined by computed tomography with similar findings. With the impression of bilateral neuroblastoma or metastatic spread, the laparotomy was performed on the 13th day of life. Frozen section of biopsy of the left neck mass was obtained, which showed neuroblastoma. Intraoperative findings revealed bilateral adrenal masses which were distinct and anatomically separate. Bilateral adrenalectomy was accomplished and the initial postoperative course was unevenful. The patient was discharged for hopeless and expired at age 45 days. We present bilateral adrenal neuroblastoma considered to be simultaneous occurrence rather than metastases from one site to another.

