Early suspicion is essential in diagnosing pyriform sinus cysts. We report two neonatal cases of pyriform sinus cysts presented as neck masses. The first case presented as a right neck mass, which made it more difficult to suspect a pyriform sinus cyst considering the prevalence of left sided cysts. Surgical resection was done in both cases and anatomical investigation suggested both to originate from the fourth branchial pouch. Detection of air bubble containing mass on imaging studies can aid early diagnosis and early use of gastric tube feeding can facilitate treatment by preventing milk contamination which may result in infection of the sinus cyst.
This study aimed to evaluate the relationship between nutritional support and growth velocity after abdominal surgery in neonates.
The electronic medical records of 45 neonates who underwent abdominal surgery in neonatal intensive care unit from 2012 to 2016 were collected to see how surgery and postoperative nutrition affect for the growth of neonate with abdominal surgery. The growth velocity was measured from the time of surgery to the time of discharge based on body weight.
In neonates who achieve their protein requirement on the first day after surgery, the growth velocity was better than that in neonates who did not achieve their protein requirement on the first day after surgery (4.31 vs. 15.21; p=0.004). Based on the type of surgery, length of bowel resection and surgical complications, this study showed better growth velocity in neonates who had no surgical complications (5.34 vs. 12.74; p=0.775), reoperation (5.25 vs. 22.19, p=0.987), or bowel resection (6.79 vs. 9.95, p=0.302). However, there was no statistically significant difference among these factors.
We concluded in this study that adequate protein supplement from the first day of surgery could have a positive effect on the growth velocity of neonates who underwent abdominal surgery.
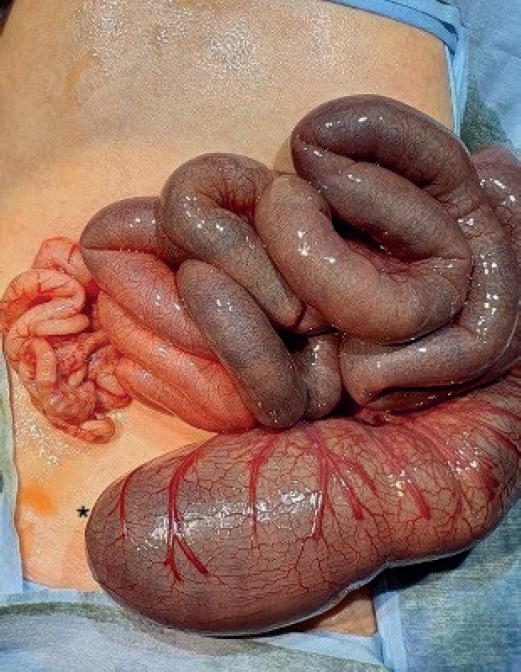
Santulli enterostomy has been used for various surgical abdominal conditions that require temporary diversion of bowel during a neonatal period. The aim of this study was to report clinical outcomes of Santulli enterostomy and to evaluate its usefulness.
Between January 2000 and December 2016, 40 neonates who underwent Santulli enterostomy were enrolled; Santulli enterostomies were performed for 25 patients without previous laparotomy (primary Santulli group) and 15 patients with previous laparotomy (secondary Santulli group).
Small bowel atresia is the first common indication of Santulli enterostomy (22/40, 55.0%), and luminal discrepancy between proximal and distal bowel was the most common determinant factor of Santulli enterostomy (17/40, 42.5%). The median age at surgery and mean birth weight were 2 days and 2,480 g respectively in the primary group, and 71 days, 2,340 g respectively in the secondary group. Operation time was significantly longer in the secondary group than the primary group (156±48 minutes vs. 224±95 minutes, p=0.019), and there was no difference in the time taken to initiation of oral feeding between the two groups. Santulli enterostomy closure was performed at median 65 days after Santulli enterostomy for primary group and 70 days for secondary group. Six complications (15.0%) were found after Santulli enterostomy, and nine complications (24.3%) after Santulli enterostomy closure (p=0.302). The incidence of complications was significantly higher in secondary group than in primary group (4.5% vs. 53.3%, p=0.001), and the reoperation rate was also significantly higher in the secondary group (4.5% vs. 46.7%, p=0.004).
Santulli enterostomy could be applied as a temporary enterostomy in neonatal patients with various surgical abdominal diseases. Considering the high complication rate after secondary Santulli enterostomy closure, decision making on the timing of enterostomy closure should be done with caution.
Spontaneous neonatal gastric perforation is a rare but fatal disease with unclear etiology. In this study, we reviewed its clinical manifestations, outcomes, and discussed the etiology and prognostic factors.
There were 12 neonates with gastric perforation in our hospital from 1989 to 2015. Their medical records were reviewed retrospectively including birth record, associated disease, site and size of perforation, type of surgical management, clinical outcome. Also, the prognostic factors were analyzed.
The median gestational age and birth weight was 32 weeks (range, 26-43 weeks; preterm birth rate, 66.7%) and 1,883 g (range, 470-4,400 g), respectively. Five patients had associated gastrointestinal anomalies including esophageal atresia and tracheoesophageal fistula (two patients), midgut volvulus, non-rotation and microcolon, and meconium plug syndrome. The median age at surgery was six days after birth (range, 2-13 days), and the median weight at surgery was 1,620 g (range, 510-3,240 g). Upper third part of stomach was the most frequently involved location of perforation. The size of perforation varied from pin point to involving the whole greater curvature. Primary repairs were done in seven cases, and in five cases, resections of necrotic portion were needed. Mortality rate was 33.3% (n=4), morbidity (re-operation) rate was 16.7% (n=2). The causes of death were sepsis (n=3), and heart failure from Ebstein anomaly (n=1). The median hospital stay was 92.5 days (range, 1-176 days). The factors mentioned as prognostic factors in previous studies showed no significant relations to the mortality and morbidity in our study.
There were improvements of outcomes in patients with large size perforation. As previous studies, we assume these improvements were possible due to the improvements of critical care medicine. Given that rare incidence, a multi-center study can help us get a better understanding of this disease, and a better outcome.
We report a neonatal case of “intraluminal” pyloric duplication cyst, causing gastric obstruction after birth. Endoscopy revealed a submucosal cystic lesion approximately 15 mm in size arising from the anterior and inferior surfaces of the pylorus obliterating the pyloric canal. After laparotomy, intraoperative cholangiography was performed, which documented no communication between the cyst and the bilio-pancreatic duct. Gastrotomy was performed transversally over the antrum, and the cyst delivered through the incision. The cyst was incised, the upper part of the cyst wall removed, and a mucosectomy performed on the inner cyst wall of the lower part. The mucosa and muscle of the margin of the cyst were approximated. At follow up of 10 months, the patient is well without any sign of gastric obstruction.
National survey for newborns surgery with congenital anomalies by Korean Association of Pediatric Surgeons (KAPS) was done. A questionnaire was sent to all members of the KAPS on March 2014. The current survey is to review three years status of the newborn surgery from 2012 to 2013. Thirty-four members (27.9%) took part in the survey that included data for the diagnosis, number and procedures of neonatal surgical cases. The result was discussed at the Topic Discussion section of the 30th Annual Congress of KAPS, 2014.
The duplication of gastrointestinal tract has been known to be a rare condition and two different forms, cystic and tubular type. This study was conducted to examine its clinical characteristics, especially cystic enteric duplication which was detected antenatally or postnatally.
There were 13 patients, who confirmed as cystic enteric duplication after operation between July 1996 and June 2015. Clinical data, including a gender, age at operation, presenting symptoms, diagnostic modalities, locations of lesion, and results of surgical treatment, were reviewed retrospectively according to cases detected antenatally and postnatally.
Five cases were included in antenatal diagnosis group and 8 cases in postnatal diagnosis group. Both groups show slightly common in female and the lesion most common in ileum. Antenatal diagnosis group shows 2 males and 3 females and the mean age at operation was 12±52 days (range, 5 to 90 days). They received operation regardless of symptom. Postnatal group shows 3 males and 5 females and the mean age at operation was 462.5±777.0 days (range, 4 days to 6 years). Moreover, 6 patients (75.0%) were age before 2 years. They usually presented abdominal pain with vomiting.
Cystic enteric duplication could present symptoms at any time during childhood, mainly before 2 years old, and so a proper management should be considered when suspect it. Although it is uncommon, surgical management including a minimal invasive procedure could be attempted despite the neonatal period.
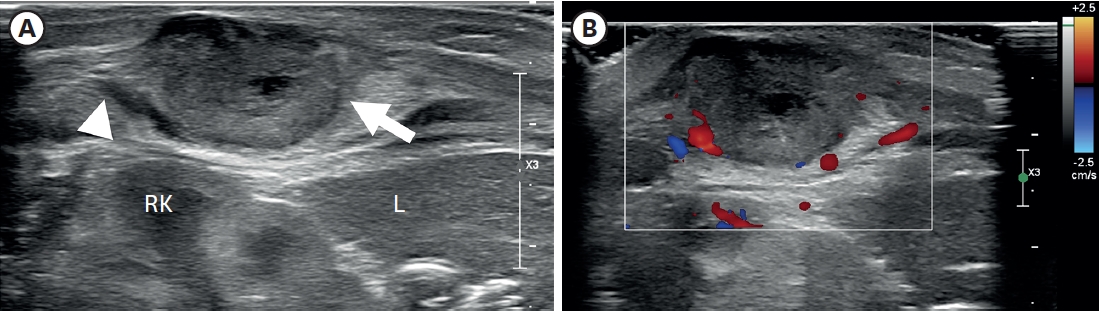
Neonatal neuroblastoma (NBL) is the most common malignant tumor in neonates, but there have been few studies about it. The purpose of this study was to investigate the clinical features of NBL and to compare prenatal and postnatal diagnosed groups.
Nineteen patients who were diagnosed with NBL prenatally or within 28 days after birth from February 1986 to February 2013 in Seoul National University Hospital were enrolled in the study. The patients were categorized according to the International Neuroblastoma Staging System (INSS) and Children's Oncology Group (COG). Retrospective medical-record reviews were performed on these patients. The operative date, complication, pathological stage, and overall survival of the prenatally diagnosed group and the postpartum diagnosed group were compared.
Tumor was detected via prenatal ultrasonography in 8 patients (42.1%), and 11 patients (57.9%) were diagnosed within 28 days after birth. Based on INSS, the patients were divided into the stage I (n=8), stage II (n=1), stage III (n=3), stage IV (n=4), and stage IVs (n=3) groups, respectively. Based on COG, on the other hand, the patients were divided into the low-risk (n=8), intermediate-risk (n=8), and high-risk (n=3) groups. The postoperative complication rate was 29%. One patient died from complications from chemotherapy. The other 18 patients' mean follow-up period was 77.7 months. The differences between the postoperative complication rate, proportion of early-stage tumor, and overall survival of the prenatal and postnatal groups were not statistically significant (p=0.446, p=0.607, p=0.414).
NBL showed favorable outcomes but relatively higher postoperative complications. There seem to be no significant statistical differences in the postoperative complications, proportion of early-stage tumor, and overall survival between the prenatally diagnosed group and the postpartum diagnosed group.
Acute appendicitis is very rare in premature neonates. Preoperative diagnosis of this condition is difficult, and then it leads to high morbidity and mortality. We report 9-day-old premature male with ruptured acute appendicitis presented with pneumoperitoneum on plain films of the abdomen. Awareness of this rare condition and possible differential diagnosis in this age group is also discussed.
Meconium obstruction (MO) in neonates arises from highly viscid meconium and the poor motility of the premature gut. Recently the incidence of the MO in neonates has been increasing, but, the diagnosis and treatment of this disease have not yet been clarified. Between March 2004 and April 2010, 24 neonates were treated for MO at Severance Children's Hospital. Their clinical characteristics and treatment were reviewed retrospectively. Twenty neonates were diagnosed with MO and 4 neonates were diagnosed with Hirschsprung's disease (HD). The mean birth weight and gestational age of the 20 neonates with MO were 1.45±0.90kg and 31.1±4.6 weeks, respectively. Thirteen neonates (65%) diagnosed with MO weighed less than 1.5kg and 10 neonates (50%) weighed less than 1kg. Half of the neonates with MO were treated by non-operative methods and the other half were treated by operative methods. Compared with the group that weighed over 1.5kg, the group that weighed less than 1.5kg were more frequently operated upon (61.5% vs. 28.5%), and contrast enemas were performed later and more frequently. Also the group that weighed less than 1.5kg had a higher mortality rate (15.4% vs. 0%). Three of the four neonates with HD were diagnosed with long-segment aganglionosis. In conclusion, MO occurred in very low birth weight neonates more often and must be differentiated from HD. Also, MO in very low birth weight neonates should be treated with special attention due to more a complicated clinical course.
There are considerable controversies in the management of congenital diaphragmatic hernia. By 1997, early operation, routine chest tube on the ipsilateral side and maintainingrespiratory alkalosis by hyperventilation were our principles (period I). With a transition period from 1998 to 1999, delayed operation with sufficient resuscitation, without routine chest tube, and permissive hypercapnia were adopted as our practice. High frequency oscillatory ventilation (HFOV) and nitric oxide (NO) were applied, if necessary, since year 2000(period II). Sixty-seven cases of neonatal Bochdalek hernia from 1989 to 2005 were reviewed retrospectively. There were 33 and 34 cases in period I and II, respectively. The neonatal survival rates were 60.6 % and 73.5 %, respectively, but the difference was not significant. In period I, prematurity, low birth weight, prenatal diagnosis, inborn, and associated anomalies were considered as the significant poor prognostic factors, all of which were converted to nonsignificant in period II. In summary, improved survival was not observed in later period. The factors considered to be significant for poor prognosis were converted to be nonsignificant after change of the management principle. Therefore, we recommend delayed operation after sufficient period of stabilization and the avoidance of the routine insertion of chest tube. The validity of NO and HFOV needs further investigation.
Gastric perforation of newborn is a rare, serious, and life threatening problem. The pathogenesis of gastric perforation is less well understood, and ranges widely. That ischemia is responsible for intestinal perforation enhances the likelihood that a similar mechanism exists for gastric perforation. Twelve patients with neonatal gastric perforation who were treated upon at the Department of Pediatric Surgery, Hanyang University Hospital from 1987 to 2002 were reviewed. Eight patients were male and four female. The age of perforation was 1 day to 8 days of life. Ten patients undertook operation and 2 patients were treated conservatively. The perforation site was located at the anterior wall along the greater curvature of the stomach in 8 patients and along the lessor curvature of the stomach in 2. The precipitating factors were gastroschisis, premature baby on ventilator and mechanical intestinal obstruction each 2 cases, and cyanotic heart disease and indomethacine medication each one case. In 5 cases the cause of perforation was not identified. The mortality rate was 25%(3 of 12). Earlier recognition and treatment were throught to be crucial prognostic factors.
Spontaneous gastric perforation in the newborn is a rare disease that requires early diagnosis and prompt surgical treatment. Between 1988 and 2001 at the Department of Pediatric Surgery, Kyungpook National University Hospital, 9 cases of spontaneous gastric perforation were treated. Seven were males and two females. The mean gestational age and birth weight were 36.7 weeks and 2,455 grespectively. All patients presented with severe abdominal distention and pneumoperitoneum on cross table lateral film of the abdomen. Perforations were located on the anterior wall along the greater curvature of the stomach in six and on the posterior wall along the greater curvature in two. One case showed two sites of perforation on the anterior and posterior wall along the greater curvature. Six patients were managed with debridement and primary closure and the others with debridement and partial gastrectomy. Peritoneal drainage was not performed. There were four deaths; two from sepsis due to leakage from the anastomotic site, one as a result of acute renal failure, and the other by associated respiratory distress syndrome. Spontaneous gastric perforation in the newborn is usually located along the greater curvature. Elevated intragastric pressure is a possible cause of the perforation. Poor prognosis is related to associated diseases and prematurity.
Multisystem organ failure resulting from gram negative bacterial sepsis is associated with high morbidity and mortality in surgical neonates. There are differences in the clinical characteristics of organ failure in neonates and adults. The purpose of this study is to identify the differences and determine the order of organ failure between baby rats and adult rats after induction of gram negative sepsis. Fifty baby rats less than 30-day-old and another 50 adult rats more than 2-month-old were divided into control group (G1) and experimental group (G2). The G1 consisted of 10 baby- and 10 adult-rats, and the G2 consisted of 40 babies and 40 adults. E. coli (108/mL per 100g of body weight) were injected into the peritoneal cavity in G2 and same amount of saline was injected in G1. Blood samples were obtained before injection, 24 hour, 48 hour, 72 hour and after death. WEC, platelet, PaO2, PaCO2, total bilirubin, BUN, creatinine, albumin and abdominal wall thickness were measured to evaluate the sequence of organ failure. The mortality was 55.0 % in G2-babies and 32.5 % in G2-adults. In baby rats, microvascular, hematologic and renal failure appeared within 24 hours after injection and pulmonary failure followed. Pulmonary, renal and liver failure developed within 24-48 hours in adult rats; however, microvascular failure did not appear until they were moribund. Thrombocytopenia, hypoalbuminemia, increased BUN and generalized edema was the earlist sign of sepsis in baby rats.
To estimate the normal anal canal pressure in neonates, anal manometry was performed in 46 normal babies less than 6 days of age. Twenty-eight of the subjects were boys and 18 girls. All the subjects passed meconium within 24 hours after birth. Birth weights were above 2.4 kg. There were no sexual differences in birth weight, birth height, gestational age, postnatal age, or Apgar score (p<0.05). The mean manometry values were; anal sphincter length 18.6± 3.9 mm, high pressure zone (HPZ) 9.2 ± 3.6 mm, vector volume 2027.2 ± 2440.7 mmHg2cm, maximum pressure 42.3 ± 17.4 mmHg, and position of the maximum pressure 6.0 ± 22.4 mm. Only the HPZ of boys was longer than those of girls (p=0.005). In squeezing state, HPZ and the position of maximun pressure were not changed from resting state. HPZ, vector volume, and maximum pressure in boys were higher than those in girls. As the birth weight increased, the anal sphincter length (p=0.001) and the HPZ increased (p=0.047). The resting pressures of the anal canal were evaluated in three portions; /23 upper portion, 12.8± 8.6mmHg, middle portion, 20.3 ± 10.8mmHg, and lower portion, 26.1 ± 12.9 mmHg. These normal values may serve as guidelines for the evaluation, diagnosis and treatment of neonatal anal diseases.
Diagnosing Hirschprung's disease is one of the clinical challenges of this disorder. In the stomach and the intestines, Cathepsin D was readily detected in cytoplasm of the rat gastric and in intestinal ganglion cells of the autonomic nervous system. The
objective
s of the present study were to examine cathepsin D expression in ganglion cells of the submucosal and myenteric plexuses of the intestine of children and to determine the utility of immunohistochemical staining of cathepsin D for detection of immature ganglion cells. Paraffin blocks of 35 intestinal segments were reviewed for immunohistochemical staining with polyclonal antibody to cathepsin D and hematoxylineosin stainings from the compatible specimens. There were 9 aganglionic segments and 9 ganglionic segments of neonates with Hirschsprung's disease, 8 intestinal segments with non-Hirschsprung's disease in neonates and 9 intestinal segments with non-Hirschsprung's disease infants over the age of 10 months. All ganglion cells showed intense granular cytoplasmic reactivity for cathepsin D regardless of maturity and all aganglionic segments had no expression for cathepsin D in the submucosal and myenteric plexuses of the intestine. However, histiocytes within the laminar propria and submucosa stained positively for cathepsin D. In conclusion, intestinal ganglion cells in children have reactivity for cathepsin D, threrfore immunohistochemical staining for cathepsin D can be used for identification of ganglion cells in neonates.
Parenteral nutntlon has been an essential part of postoperative care of neonates requiring major surgery who are unable to tolerate enteral feeding for long periods during the postoperative period. However, TPN via central venous catheters(central TPN), used in increasing trend, still presents significant morbidity. To find out whether TPN via peripheral veins(peripheral TPN) could be used as a viable alternative for postoperative parenteral nutrition in neonates, a clinical study was carried out by a retrospective analysis of 53 neonates subjected to peripheral TPN for more than 7 days after surgery. Operations consisted of procedures for esophageal atresia with tracheoesophageal fistula, gastroschisis and omphalocele. Surgery was performed at the Division of Pediatric Surgery, Department of Surgery, Hanyang University Hospitall, from 1983 to 1994. The mean total duration of TPN was 13.3 days (range; 7-58 days), the average daily total fluid intake was 117.6 ml/kg during TPN and 158.6 ml/kg during subsequent oral feeding. The average daily total calorie intake was 57.7 kcal/kg during full strength TPN and 101.3 kcal/kg during subsequent oral feeding. The mean urine output was maintained at 3.5 ml/kg/hour during TPN and at 3.6 ml/kg/hour during subsequent oral feeding. The increment of body weight observed during TPN was 132g in TEF, 53g in gastroschisis and 3g in omphalocele patients, while loss of body weight was not observed. The mortality rate was 5.7%(3/53) and was related to the underlying congenital anomalies, not the TPN. The most common complication of peripheral TPN observed was laboratory findings suggestive of liver dysfunction in 23 cases( 43.4%) with no significant clinical symptom or signs in any case, transient pulmonary edema in one case, and generalized edema in one case. None of the major complications usually expected associated with central TPN were observed. The result of this study suggest that peripheral TPN can be used for adeguate postoperative nutritional support in neonates requiring 2 to 3 weeks of TPN.
Appendiceal perforation is uncommon in the neonate. Diess reported the firs case in 1908. Approximately HI additional cases have been reported since that time. However, with exclusion of neonatal appendicitis' associated with inguinal or umbilical hernias, n,ecrotizing enterocolitis, meconium plug, and Hirschsprung's disease, there are only 36 cases of primary neonatal appendicitis. We treated a 12 days old boy with perforation of the appendix. The infant was 3000 g at birth and had a normal spontaneous vaginal delivary at 35 weeks of gestation. The mother was 31-year-old and had premature rupture of membrane. After normal feeding for the first 5 days of life, the infant had emesis of undigested milk, decreased activity and jaundice. The baby was admitted to the Pediatrics. Progressive abdominal distension, fever, decreased activity, and vomitting developed over the next six days. Erect abdominal radiography showed pneumoperitoneum. At exploratory laparotomy, a 0.8 × 0.6 em sized perforation was noted at antime-senteric border of midportion of the appendix. Trasmural inflammation and the presence of ganglion cells were noticed on histology.
Perforation of the gastrointestinal tract in neonatal period has been associated with a grim prognosis. Recently there has been some improvement in survival. To evaluate the remaining pitfalls in management, 19 neonatal gastrointestinal perforation cases from May 1989 to July 1996 were analysed retrospectively. Seven patients were premature and low birth weight infants. Perforation was most common in the ileum{56.3%). Mechanical or functional obstruction distal to the perforation site was identified in 7 cases; Hirschsprung's disease 3, small bowel atresia 3, and anorectal malformation 1. These lesions were often not diagnosed until operation. Five cases of necrotizing enterocolitis and 1 of muscular defect were the other causes of perforation. In six cases, the cause of the perforation was not identified. Perinatal ischemic episodes were associated in five cases. Overall mortality was 15.1 %. Because a considerable number of gastrointestinal perforations resulted from distal obstruction, pediatric surgeon should be alert for early identification and intervention of gastrointestinal obstruction, particularly in patients that are premature and have a history of ischemia..
Spontaneous gastric perforation is an important but rare cause of gastrointestinal perforation in neonates. Just over 200 cases have been reported in the literatures. In spite of recent surgical advances in its managements, mortality rate has been reported as high as 25~50%. Because of physiologic differences, immature immune mechanisms, variations in gastrointestinal flora and poor localization of perforation, a neonate with gastric perforation is at high risk. The pathogenesis is greatly debated. Five patients with spontaneous neonatal gastric perforation who were operated upon at the Department of Pediatric Surgery, Seoul National University Hospital from 1980 to 1993 were reviewed. Four patients were male and one female. The first indication of perforation was 1 day to 6 days of life. All of 5 perforations were located along the greater curvature of the stomach. The size of perforation ranged from 2 cm to 10 cm. Debridement and primary closure were performed in all patients. The operative mortality was 40%(2 of 5). The cause of perforation was not identified in all cases. Prematurity and necrotizing enterocolitis, synchronous or metachrotlous, were thought to be crucial prognostic factors. Earlier recognition and surgical intervention are necessary to reduce morbidity and mortality.
Primary segmental volvulus of the small intestine is not associated with malrotation, malfixation of the midgut, nor other primary small bowel lesions such as small bowel tumors. This entity is known to be more prevalent in adult and in certain global areas associated with particular diet habits. There have been very few reports in neonates, but not in this country so far. The author reports two cases of primary segmental volvulus. Case 1 was a septic 4-day-old girl with hematochezia due to jejunal volvulus with partial necrosis and panperitonitis. Resection of the segment and Bishop-Koop enterostomy were successful. Case 2 was a 3-day-old boy, who had ileal volvulus with ultra-short length of ileal atresia, probably due to intrauterine segmental volvulus. Limited resection of the atresia and spreading of the mesenteric base were enough to recovery. The rarity of the pathognomonic findings and limitation of the diagnostic workup due to rapid prqgression limit early diagnosis and good survival rate in this particular condition.
Neonatal intestinal perforation is mainly caused by necrotizing enterocolitis, intestinal atresia, meconium ileus or unknown etiology. Occasionally, Hirschsprung's disease presents with neonatal intestinal perforation, of which, it is known that total colonic aganglionosis is common. Therefore, Hirschsprung's disease should be considered as a cause of neonatal intestinal perforation.
The authors have experienced 3 cases of neonatal Hirschsprung's disease associated with colonic perforations. Cecal perforations were noted in 2 cases with aganglionosis from descending colon and sigmoid perforation in a case with aganglionosis in rectum. These cases will be discussed with literature review.

