Hepatocellular carcinoma (HCC) is a rarely occurring disease in the pediatric population. We report our center's experience of management of HCC in children and adolescents.
From 1996 to 2012, 16 patients aged 18 or younger were diagnosed with HCC at our center. The medical records of these 16 patients were retrospectively reviewed.
There were 9 boys and 7 girls. Median age at diagnosis of HCC was 14.5 years. All patient had pathologically confirmed diagnosis of HCC. Three patients had distant metastasis at the time of HCC diagnosis. Eight patients were surgically managed, including 4 liver resections, 3 liver transplantations, and 1 intraoperative radiofrequency ablation. The remaining 8 patients received systemic chemotherapy. Overall, 6 patients are alive at median 63.6 months after diagnosis of HCC. All survivors were surgically managed patients.
HCC is a rare disease occurring in childhood. Patients with systemic disease have poor outcome. Liver transplantation may be a good option for treatment of pediatric HCC.
The purposes of this study was to describe the clinical correlation of mass size and gestational age, prognostic factors in sacrococcygeal teratoma (SCT) at a tertiary pediatric surgery, University of Ulsan College of Medicine and Asan Medical Center (AMC), Seoul, Korea. Fifty five patients admitted to the AMC with a SCT between May 1989 and April 2013 were included in this retrospective review. Mean follow up was 861 days. Mean maternal age at delivery was 30 ± 2.7 year, mean gestational age (GA) was 36.9 ± 3.6wks, and preterm delivery was 21.8%. Birth body weight was 3182 ± 644 g and male vs. female ratio was 1:2.05. We can't find significant difference between Caesarean section and maternal age at delivery (
Citations

Pediatric liver transplantation has evolved into a definite and effective therapeutic modality for various liver diseases in the pediatric patient. During the last 25 years, liver transplant outcomes in Korea have reached international standards and Korea has become the leader in living-donor liver transplantation. This review will present the cumulative outcomes of pediatric liver transplantation performed in Korea and will focus on other issues of interest involving pediatric liver transplant recipients, especially in the field of immunosuppression and post-transplant lymphoproliferative disease.
Citations

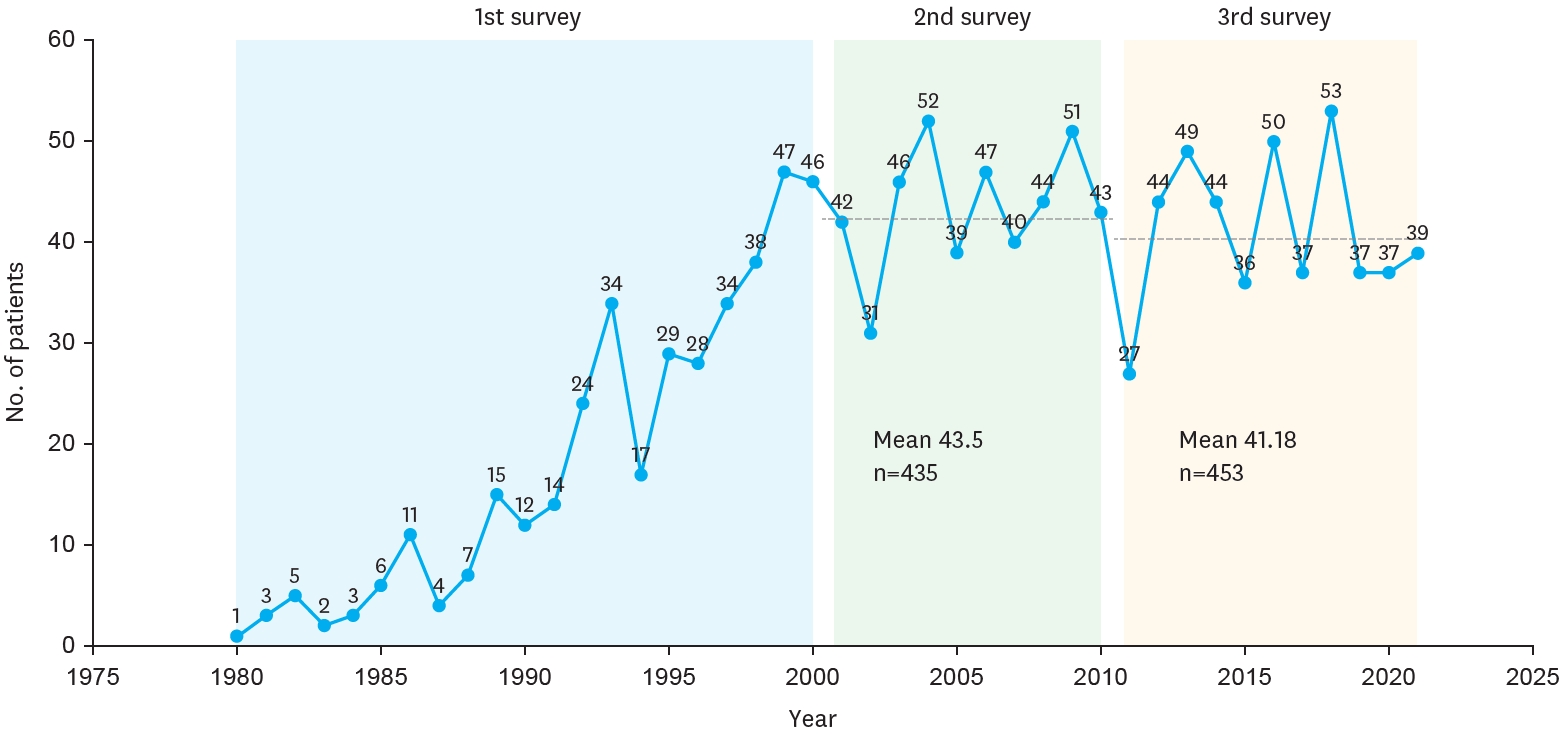
The Korean Association of Pediatric Surgeons (KAPS) performed the second nationwide survey on biliary atresia in 2011. It was a follow-up study to the first survey, which was performed in 2001 for the retrospective analysis of biliary atresia between 1980 and 2000. In the second survey, the authors reviewed and analyzed the clinical data of patients who were treated for biliary atresia by the members of KAPS from 2001 to 2010. A total of 459 patients were registered. Among them, 435 patients primarily underwent the Kasai operation. The mean age of patients who underwent the Kasai operation was 66.2±28.7 days, and 89.7% of those patients had type III biliary atresia. Only five patients (1.4%) had complications related to the Kasai operation. After the Kasai operation, 269 (61.8%) of the patients were re-admitted because of cholangitis (79.9%) and varices (20.4%). One hundred and fifty-nine (36.6%) of the patients who underwent the Kasai operation subsequently underwent liver transplantation. The most common cause of subsequent liver transplantation was persistent hyperbilirubinemia. The mean interval between the Kasai operation and liver transplantation was 1.1±1.3 years. Overall the 10-year survival rate after the Kasai operation was 92.9% and the 10-year native liver survival rate was 59.8%. We had 23 patients for primary liver transplantation without the Kasai operation. The mean age patients who underwent primary liver transplantation was 8.6±2.9 months. In summary, among the 458 Kasai-operation and liver-transplantation patients, 373 lived, 31 died, and 54 were unavailable for follow up. One-third of the patient who survived have had complications correlated with biliary atresia. In comparison with the first survey, this study showed a higher survival rate and a greater number of liver transplantation.
Citations

Biliary atresia (BA) is an infantile cholestatic disease of progressive obliterative cholangiopathy with varying degrees of damage to both extra and intrahepatic bile ducts due to unknown causes. The diagnostic studies should be done to diagnose or exclude BA without unnecessary delay. Kasai portoenterostomy is the first choice of treatment for bile drainage from microscopic bile ductules present in the portal fibrous mass. The medical management after Kasai portoenterostomy should be done carefully to maintain bile excretion and prevent and treat complications including cholangitis, hepatic fibrosis, portal hypertension and nutritional problem. The reported five years-survival rates after Kasai portoenterostomy range from 30 to 60%. About 20% of all patients undergoing Kasai portoenterostomy during infancy survive into adulthood with their native liver. Even if Kasai portoenterostomy remains as the first line of treatment in BA, liver transplantation serves as a good salvage treatment when portoenterostomy fails or liver function gradually deteriorates after initially successful establishment of bile flow. Overall 5-year survival rate in BA is about 90% in recent series.
Infantile hepatic hemangioendothelioma (IHHE) is the most common benign vascular hepatic tumor in children. We analyzed the 17-year experience of IHHE. The medical records of 16 patients (M:F=8:8) treated at the Department of Pediatric Surgery and the Department of Pediatrics Seoul National University Children's Hospital between January 1991 and January 2008 were reviewed retrospectively. Mean age at presentation was 87 days (1 day-551 days). Seventy five percent of patients were diagnosed with imaging study and 25% with biopsy. Major symptoms were hepatomegaly (N=5), palpable abdominal mass (N=4) and congestive heart failure (N=3). Six patients had no symptoms. Kasabach-Merritt syndrome was combined in one patient. Nine patients (56.3%) underwent operation and 2 patients (12.5%) underwent only medical treatment. Clinical observation was tried on 5 patients (31.3%) without any treatment. Operation was performed on the patient with clinical symptoms or on patients where the differentiation between begin and malignant could not be determined. Patients who had clinical symptoms but tumor was unreresectabile were treated medically. Among the 5 patients who had been observed for their clinical course, 2 patients showed complete regression and the tumors of the remaining 3 patients were regressing. Clinical symptoms, the age at presentation, the size of tumor and α-FP, all had no significant statistical relationship with the time required for complete tumor regression. There was no relationship between the size change of the tumor and the change of α-FP level. Only the size of tumor was related with clinical symptoms. One patient died of post-operatvie bleeding. Treatment plan was determined by the extent of the tumor and the presence of clinical symptoms. Observation was enough for the patients without clinical symptoms and complete resection was curative for patients with clinical symptoms. Medical treatment is an alternative for the patient whose tumor is unresectable.
Citations

Liver tumors in children are rare, relatively complex, and encompass a broad spectrum of disease processes. This study reviews our experience of liver tumors during the last 10 years. Medical records of 36 cases of liver tumors?in children, treated at Samsung Medical Centers, from October 1994 to December 2005, were reviewed in this study. We analyzed disease characters and survival rates as a whole and by specific disease. The median age was 3.6 years. Male and female ratio was 1:1. The most common symptom was the palpable mass in 15 cases. Others were abdominal distension in 9 cases, jaundice in 2, vomiting in 2, weight loss in 2, and pubic hair growth in 1. CT or US and liver biopsy were performed for diagnosis. There were 28 malignant tumors: malignant rhabdoid tumor (1 case), hepatocellular carcinoma (3 cases), hemangioendothelioma type II (3 cases), angiosarcoma (1 case), and hepatoblastoma (20 cases). Eight tumors were benign; hepatic adenoma (1 case), focal nodular hyperplasia (2 cases), hemangioendothelioma type I (2 cases), mesenchymal hamartoma (3 cases). In this study the clinical characteristics were not different from the other reports. Liver transplantation was performed in 3 cases-1 with hepatoblastoma and 2 with hepatocelleular carcinoma. Accurate and early diagnosis, and individualized multi- modality therapeutic approaches might be important for better outcome.
Citations

Solid pseudopapillary tumor of pancreas in children is a tumor with low malignant potentiality, and is rarely associated with distant metastasis. A 13-year-old girl was hospitalized because of abdominal pain of one week duration. Abdominal CT revealed not only a 12×6cm sized mass at the pancreatic body and tail but also a 1cm sized mass in left lobe of the liver. The patient underwent a near-total pancreatectomy and tumorectomy of the liver. A solid pseudopapillary tumor with liver metastasis was confirmed by pathology. She has undergone 13 courses of chemotherapy and has been well for 13 months without any sign of recurrence.
Mesenchymal hamartoma of the liver is a rare benign tumor, usually presenting in early childhood. Five children with mesenchymal hamartoma of the liver pathologically verified at Seoul National University Children's Hospital between 1978 and 2000 were analyzed retrospectively. There were two girls and three boys, and their mean age at the operation was 16.0months (range, 4 - 32 months). Three patients presented with abdominal distension. A patient was detected incidentally, and another was detected by prenatal ultrasongraphic examination. Tumor size ranged from 10x8.5cm to 34x29cm. Three tumors were located in the right lobe and two in the left lobe. Four cases underwent complete surgical resection, and the other one underwent incomplete surgical resection and marsupialization. Recurrence or malignant transformation was not noted. Five patients survived without evidence of disease for 35, 36, 38, 142 and 228 months. In conclusion, although mesenchymal hamartoma of the liver is benign lesion, it may be confused, and mixed with embryonal sarcoma. A recent report showed recurrence or malignant transformation after partial excision of the tumor. Therefore, complete excision of the tumor with surrounding normal liver tissue is recommended.
Citations

A clinical review was done of 31 children with blunt liver injury who were admitted to the Department of Surgery, Kyungpook National University Hospital , between 1981 and 1990. Seventeen of the 31 children required laparotomy(11 primary repairs, 4 lobectomies, 2 segmentectomies). There were two deaths after laparotomy, one due to associated severe head injury and another due to multiorgan failure. The remaining 14 children, who were hemodynamically stable after initial resuscitation and who did not have signs of other associated intraabdominal injuries, were managed by nonoperative treatment. Patients were observed in a pediatric intensive care unit for at least 48 hours with repeated abdominal clinical evaluations, laboratory studies, and monitoring of vital signs. The hospital courses in all cases were uneventful and there were no late complication. A follow-up computed tomography of 7 patients showed resolution of the injury in all. The authors believe that, for children with blunt liver injuries, nonoperative management is safe and appropriate if carried out under careful continuous surgical observation in a pediatric intensive care unit.