Total proctocolectomy with ileal pouch-anal anastomosis (T-IPAA) in childhood is a surgical procedure mainly applied to familial adenomatous polyposis (FAP) or ulcerative colitis (UC), but it can be applied to non-FAP/non-UC disease (NFNU). Studies regarding the role of T-IPAA who underwent the operation in childhood, especially in terms of long-term gastrointestinal function, complications, and quality of life (QOL) are limited. The aim of this study was to evaluate the characteristics of patients receiving T-IPAA and to compare their bowel function outcomes and QOL.
Patients aged ≤18 years at the time of T-IPAA were included. Their medical records were retrospectively reviewed. Krickenbeck classification, Cleveland Clinic Incontinence (CCI) score, 36-item Short-form Health Survey Questionnaire, and Gastrointestinal Quality of Life Index were used for the evaluation of bowel function and QOL. The median follow-up period was 9.8 years.
Of the 25 patients, 9 had FAP, 9 had UC, and 7 had NFNU. NFNU include 3 of Hirschsprung disease, 2 of intestinal neuronal dysplasia, and 2 of imperforate anus. The median age at T-IPAA was 17.8, 14.2, and 9.3 years for FAP, UC, and NFNU, respectively (p=0.001). Bowel function was satisfactory in terms of voluntary bowel movement (VBM), soiling, and constipation. VBM and constipation were not different between the groups, but soiling was most in NFNU (100%, p=0.047). However, QOL was best in the NFNU group in surveys (p=0.034 and 0.004, respectively).
T-IPAA could be safely applied not only for FAP and UC but also for other diseases in selective cases, with caution.
Santulli enterostomy has been used for various surgical abdominal conditions that require temporary diversion of bowel during a neonatal period. The aim of this study was to report clinical outcomes of Santulli enterostomy and to evaluate its usefulness.
Between January 2000 and December 2016, 40 neonates who underwent Santulli enterostomy were enrolled; Santulli enterostomies were performed for 25 patients without previous laparotomy (primary Santulli group) and 15 patients with previous laparotomy (secondary Santulli group).
Small bowel atresia is the first common indication of Santulli enterostomy (22/40, 55.0%), and luminal discrepancy between proximal and distal bowel was the most common determinant factor of Santulli enterostomy (17/40, 42.5%). The median age at surgery and mean birth weight were 2 days and 2,480 g respectively in the primary group, and 71 days, 2,340 g respectively in the secondary group. Operation time was significantly longer in the secondary group than the primary group (156±48 minutes vs. 224±95 minutes, p=0.019), and there was no difference in the time taken to initiation of oral feeding between the two groups. Santulli enterostomy closure was performed at median 65 days after Santulli enterostomy for primary group and 70 days for secondary group. Six complications (15.0%) were found after Santulli enterostomy, and nine complications (24.3%) after Santulli enterostomy closure (p=0.302). The incidence of complications was significantly higher in secondary group than in primary group (4.5% vs. 53.3%, p=0.001), and the reoperation rate was also significantly higher in the secondary group (4.5% vs. 46.7%, p=0.004).
Santulli enterostomy could be applied as a temporary enterostomy in neonatal patients with various surgical abdominal diseases. Considering the high complication rate after secondary Santulli enterostomy closure, decision making on the timing of enterostomy closure should be done with caution.
A nationwide survey on necrotizing enterocolitis (NEC) was undertaken among members of the Korean Association of Pediatric Surgeons. The members were required to complete a questionnaire and the case registration form for each patient during the three-year period from July 2001 to June 2004. Eighty one patients were included in the questionnaire, but only 71 patients were registered from 22 members in 16 hospitals. At the same time survey on focal intestinal perforation (FIP) was undertaken and 17 patients were registered from 11 members in 10 hospitals. Total 19,041 newborns were admitted to neonatal intensive care unit during the study period. Eighty one patients (17.27 %) were underwent surgery among 469 babies who were managed under the impression of NEC. The male to female ratio was 2.1:1. The premature were 60.6 %. The most common site of involvement was ileum. Overall and operation survival of NEC were 72 % and 79 %, respectively. The survival was lower in smaller babies, multiple segments involvement and involvement of both the small and large intestine. But there was no difference in survival according to sex or prematurity. The FIP showed very similarity with NEC in terms of incidence, and the age of diagnosis and operation. But the survival was much better and 100 %. The results showed the clinical characteristics of NEC and the trend of management in NEC in Korea. In the future we hope we can discuss about this topic in prospective manner.
performed at the time of discharge. There was only one recurrence of adirect inguinal hernia. Necrotizing enterocolitis developed in 17 patients, 11 were operated upon, two had peritoneal drainages, and 9 had enterostomies. Five of 11 surgical infants died after operation and three of the nonsurgical infants died of various complications. Although micropremies have potentially high risks of serious complications and death, the outcome can improve with careful surgical observation and judgment.
Ulcerative colitis, one of the inflammatory bowel disease, is primarily managed medically with combinations of 5-ASA and steroids. However, this chronic disease requires surgical management if symptoms persist or complications develop despite medical management. The clinical course, the indications and outcome for surgical management of pediatric ulcerative colitis patients were studied from medical records retrospectively. Twenty-one patients under the age of 15 who were endoscopically diagnosed with ulcerative colitis at the Seoul National University Children's Hospital between January, 1988 and January, 2003 were subjected to the study. Mean follow up period was 3 years and 10 months. The mean age was 10.3 years old. All patients received medical management primarily after diagnosis and 8 patients (38%) eventually required surgical management. Of 13 patients who received medical management only, 7 patients (53%) showed remission, 4 patients are still on medical management, and 2 patients expired due to congenital immune deficiency and hepatic failure owing to sclerosing cholangitis respectively. In 8 patients who received surgical management, 1 patient underwent surgery due to sigmoid colon perforation and 7 patients due to intractability of medical management. The perforated case received colon segmental resection and the other 7 patients recieved total protocolectomy with ileal pouch-anal anastomosis. One patient expired postoperatively due to pneumonia and sepsis. One patient is still on medical management because of mild persistent hematochezia after surgery. The other operated patients are showing good prognosis without any management. Pediatric ulcerative colitis patients can be surgically managed if the patient is intractable to medical management or if complications such as perforation is present. Total protocolectomy & ileal pouch-anal anastomosis is thought to be the adequate surgical method.
Necrotizing enterocolitis (NEC) is usually a disease of premature infants, but occasionally it affects the term neonate. Twenty-five infants with NEC were treated at Asan Medical Center between January 2000 and December 2002. and 13 of them were term infants. In each case, the diagnosis of NEC was established by a clinical illness fulfilling the Bell's stage II or III NEC as modified by Walsh or by surgical findings. There were six males and seven females. The birth weight was from 1,960 to 3,700 g. The age at diagnosis was from 1 to 40 days. Four patients had congenital heart disease; one of them had hypothyroidism and cleft palate. Abdominal distension was present in all, and bloody stools in four. One patient had history of hypoglycemia, three had Rota viral infection. Eight patients had leucopoenia (<5.0 × 109/L), Seven had thrombocytopenia (<100 × 109/L), and three severe thrombocytopenia (<50 × 109/L). Laparotomy was required in 10 of the 13 patients. Indications for operation in acute phase were failure to respond to aggressive medical therapy in five, and perforation in three patients. There were two late phase operation for intestinal stricture and fistula. There was no operative complications. Ten of thirteen patients survived (76.9%). Two patients died of septic complication. There was a delayed death due to heart failure. There was a significant difference in survival according to platelet count (50 × 109/L) (p<0.05). Congenital heart disease and Rota viral infection is associated with NEC in term infants and thrombocytopenia and leucopenia in the course may be surgical indications.
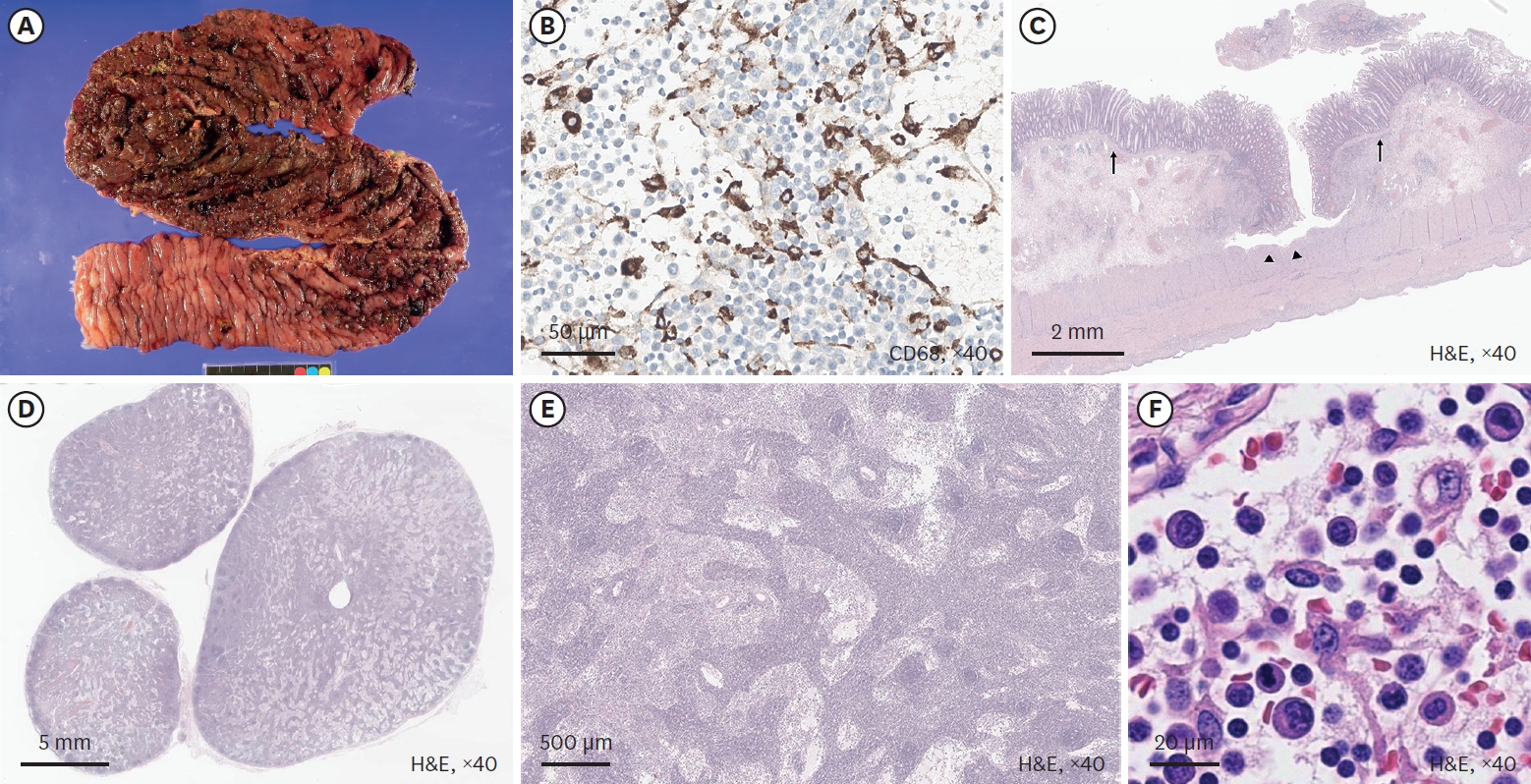
Enterocolitis associated with Hirschsprung's disease has been a major cause of morbidity and even mortality, and before and after definitieve surgical treatment. It shows typical clinical characteristics, however, its pathogenesis has been poorly understood. Treatment is diverse, and consists of conservative tertment with intravenous hydration, antibiotics and rectal wash out, and surgical tertment with temporatory enterostomy, and other surgical procedures.

